 You are entering webpages belonging to the American Association of Orthopaedic Surgeons, which includes information and resources for Association advocacy efforts and the Political Action Committee of The American Association of Orthopaedic Surgeons (OrthoPAC).
You are entering webpages belonging to the American Association of Orthopaedic Surgeons, which includes information and resources for Association advocacy efforts and the Political Action Committee of The American Association of Orthopaedic Surgeons (OrthoPAC).
The AAOS Office of Government Relations’ regulatory efforts ensure that orthopaedic concerns are addressed even after the conclusion of the legislative process and throughout agency rulemaking and implementation stages. To this end, the regulatory staff works closely with Department of Health and Human Services agencies such as the Food and Drug Administration (FDA), Centers for Medicare & Medicaid Services (CMS), the Agency for Healthcare Research and Quality (AHRQ), and the Centers for Disease Control and Prevention (CDC). In addition, expertise in coding, reimbursement, and payment policy is shared across the Academy and with our members. The Office of Government Relations also houses the AAOS’ patient safety, quality, registry and research advocacy efforts. All of these are key services to our fellowship and members.
Coding and Reimbursement
Engaged with AIM Specialty Health where they agreed that subacromial decompression (CPT code 29826) is medically necessary for some indications. The AAOS is continuing to work alongside representatives from ASES, AANA, and AOSSM to revise the guidelines to also include indications of partial bursal rotator cuff tear, subacromial impingement, and full thickness rotator cuff tear.
Received acknowledgment from the Centers for Medicare and Medicaid Services (CMS) that patient preoptimization work occurs prior to surgery for total hip and total knee arthroplasties and that this work is not currently reimbursed. AAOS and AAHKS have published interim coding recommendations and continue to develop new CPT codes and Medicare reimbursement pathways to mitigate payment cuts to these arthroplasties.
Engaged in a meeting with CMS and the National Correct Coding Initiative regarding reversing inappropriate code-pair edits and medically unlikely edits applied to orthopaedic procedures.
Presented quarterly educational webinars for members, including: CPT CMS Updates 2021, TKA & THA RVUs Impacted by 2021 CMS Final Rule, and Prior Authorizations – Peer to Peer Review. Developed online resources to support
appeals of inappropriate denials for TKA and Shoulder Arthroscopy denials.
Devices
Supported the proposal for the Medicare Coverage of Innovative Technology pathway, which would provide four years of automatic Medicare coverage for FDA-approved Breakthrough Devices. Implementation of the pathways has been delayed by the U.S. Department of Health and Human Services until December 15, 2021.
MIPS Value Pathways
Submitted two candidate MIPS Value Pathways (MVPs) to the Centers for Medicare and Medicaid Services (CMS) in February 2021. One candidate MVP focused on rotator cuff repair and utilized feedback from the Shoulder and Elbow Registry Steering Committee and the AAOS Public Advisory Board. The second candidate MVP was on lower extremity joint replacement and was a collaborative effort between AAOS surgeon members and the American Society of Anesthesiologists. CMS touts MVPs as a way to reduce reporting burden of the traditional Merit-based Incentive Payment System (MIPS) program and encourage transition to Advanced Alternative Payment Models.
- AAOS staff partnered with the American Association of Orthopaedic Executives to produce a webinar on the changes to the Quality Payment Program for 2021 & beyond, including implementation of MVPs.
- AAOS staff met with CMS to discuss candidate MVP feedback in April and June 2021. AAOS has been invited to join the MVP Strike Force group by the AMA.
- An LEJR MVP similar to the candidate submission is proposed in the first wave of reportable MVPs beginning January 1, 2022.
Orthopaedic Advocacy Week Event, May 24-28, 2021
Orthopaedic Advocacy Week was created at the request of the AAOS Presidential Line. Each day of the first-ever completely virtual event utilized a tactic in AAOS’ advocacy strategy toolbox for shaping healthcare policy and delivering critical messages to lawmakers: Growing Support with Grassroots, Amplifying our Message with Social Media, Shaping Policy through Rulemaking, a Virtual Capitol Hill Day with Lawmakers, and Getting Invested with the Orthopaedic PAC. In addition to the results listed in the graphic below, 249 members participated in the event from 39 states and Puerto Rico. Importantly 109 new legislative cosponsors were generated for bills to reform prior authorization, expand telemedicine services, and prioritize physician mental health.
Learn more about the event. 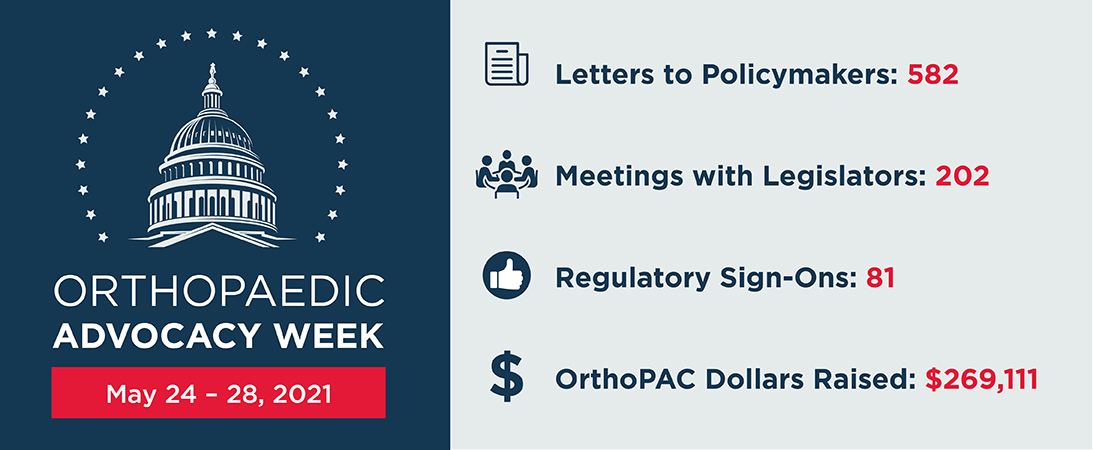
Registries
In addition to delaying the Qualified Clinical Data Registry measure testing requirements that were to come into effect January 1, 2021, AAOS successfully urged CMS to push back the 2019 MIPS data submission deadline.
Value-Based Care
Developed a value-based care continuum (VBCC) to help orthopaedic practices better understand and navigate various alternative payment models created to achieve value-based care.
Learn more and download the VBCC.
Also, completed a membership-wide Value-Based Care Survey to gather critical data on member participation in federal and commercial payer alternative payment models.