Orthopaedic surgeons often perform procedures for which no specific Current Procedural Terminology (CPT) exists. For example, hip surgeons often are frustrated that there are no codes for periacetabular osteotomy (PAO) or labral reconstruction.
“Now that orthopaedic surgeons are experienced with basic hip arthroscopy techniques, many are doing more advanced surgeries,” said orthopaedic surgeon Michael R. Marks, MD, MBA, a senior consultant with KarenZupko & Associates, Inc. (KZA).
“And many of these procedures don’t have specific CPT codes,” he added.That means physicians must understand payer authorization and coverage policy issues.
Avoid reporting codes that are ‘close enough’
According to Dr. Marks, there is a right way and a wrong way to code for an unlisted procedure.
“I’m often asked, ‘If there’s not a code that fully describes what I’m doing, but I find one that’s close enough, can I bill it so I can get paid?’” The answer is no, he said. “Choosing a code that is similar but not accurate in order to get paid is not the right thing to do. Unless the procedure you perform is specifically described in the CPT code, you must use an unlisted code.”
Instructions for use of the CPT codebook clearly state, “Select the name of the procedure or service that accurately identifies the service performed. Do not select a CPT code that merely approximates the service provided. If no such specific code exists, then report the service using the appropriate unlisted procedure or service code.”
Many surgeons are hesitant to bill for unlisted services out of fear that the procedures will be poorly reimbursed—if at all. Dr. Marks warned that following the adage “close enough is good enough” may lead to legal problems with insurers, as inaccurate coding may be considered fraud, abuse, or a false claim.
Transparency is important
For many procedures that require the use of unlisted codes, “When a practice inquires whether an authorization is needed for an unlisted code, the payer will say ‘no’ because the code isn’t in their system,” explained Cheyenne Brinson, CPA (inactive), MBA, a consultant with KZA. “The physician does the surgery, and then payment gets denied due to it being deemed experimental/investigational or lacking medical necessity.”
In the case of advanced hip procedures, attempting to obtain prior authorization for physician fees will most likely be unsuccessful because, currently, many are noncovered procedures, although many carriers may cover facility fees and inpatient stay services associated with such surgeries.
Ensuring that surgeons are paid for such procedures requires practice teams to thoroughly educate patients that unlisted procedures are not currently covered by insurance. Staff also should educate patients about their anticipated financial responsibilities, obtain waivers of understanding, and collect appropriate payments from patients. A financial counselor typically performs those tasks.
Dr. Marks advised having such conversations on the front end and collecting patients’ financial responsibilities before surgery. “Lack of transparency will cause reputational damage for hitting patients with surprise bills,” cautioned Dr. Marks.
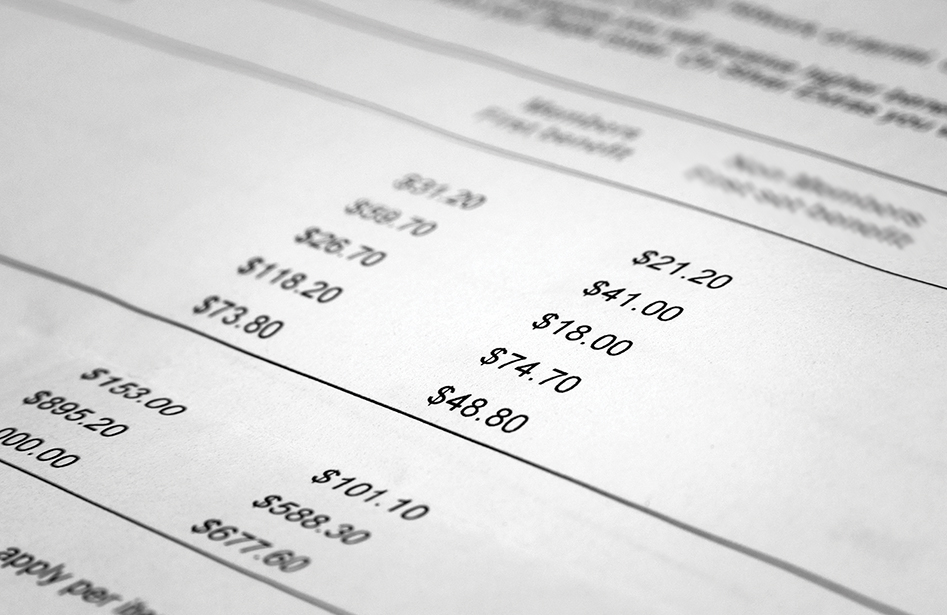
“Our financial counselors begin educating the patient as soon as the physician recommends a treatment,” said Jessica Whitten, CPC, CPPM, a practice administrator at Nashville Hip Institute (NHI). “They provide the patient with five items in a financial packet.” The packet includes a letter explaining the anticipated procedures; a financial breakdown that shows fees, out-of-pocket expenses, and how the financial counselor came up with the numbers; a waiver; a CareCredit patient financing estimate; and a copy of the patient’s benefits.
The NHI team explains to patients how payments for combination surgeries work and their financial responsibilities: “We explain the difference between a listed code and one that is unlisted. We ensure that in our discussion and paperwork these remain separate for educational purposes, and we collect on the full estimated out-of-pocket costs.”
To reassure patients that the practice has done everything possible, the NHI team attempts to obtain prior authorization on their behalf. “It’s about managing patient perception and expectations,” said Ms. Whitten. “We take a customer-service approach that shows the patient we have done our due diligence on their behalf.”
If a procedure is denied authorization, “The patient has a reference number and can call the payer to hear it for themselves if they want to. That increases their comfort level and trust in us,” she said, noting that the team also provides names and contact information for hospital billing department staff so patients can validate that a plan will cover the hospital services.
In rare cases, NHI attempts to obtain a letter of predetermination from a payer. “This is a last-ditch effort on our part,” said Ms. Whitten, adding that this route takes additional physician time and requires at least 30 days for a response. “We’ve never been successful [in] getting predetermination approval for PAO or labral reconstruction,” she said.
Waivers are essential
A signed waiver indicates that you have explained to a patient that he or she will be responsible for payment and, more importantly, that he or she accepts responsibility for payment. Medicare patients must sign an advanced beneficiary notice when services are not covered.
“Generally speaking, commercial carriers don’t require a similar waiver,” Dr. Marks said.
According to Ms. Whitten, only a few of NHI’s commercial plans have preferred waivers. The practice has developed its own waivers for the others. Recently, a payer contacted NHI asking to see a signed patient waiver for a noncovered service. Ms. Whitten sent it to show the patient’s signature, indicating that the patient understood that the procedure was not covered. “The waiver is crucial to show that you’ve documented patient education,” she said.
Offer multiple payment options
Most patients do not have cash on hand to cover the costs of advanced hip procedures in one payment. Offering patients multiple payment options is important.
There are two collection techniques to consider. One involves automated, recurrent payments on a credit card. The other is patient financing. Ms. Whitten said financing gives patients the purchasing power to schedule services and surgeries quickly. “We offer financing to every patient, not just as a final option to those who can’t pay using other means,” she explained. The 12-month, deferred interest program has been popular. “Having a full year to make payments without interest is very attractive when patients are considering surgery,” Ms. Whitten said.
Documentation tips
Although advanced hip procedures currently are not covered, it is important to bill such cases and post denials into your computer system.
Staff should refer to proposed codes in prior authorization letters and use them to complete claim forms. Report an unlisted code only once. “Doctors will often report multiple unlisted codes,” said Dr. Marks. “But the payer only wants it once on the claim. Often, payers reject claims when multiple unlisted codes are reported.”
Claims for unlisted codes can be submitted electronically with operative notes and prior authorizations attached. “In the past, unlisted codes had to be billed on paper,” explained Dr. Marks. “Now, most payers want you to submit the claim and your operative note electronically. It’s a lot more efficient.”
In the operative note, “Include the details of how you met medical necessity, surgical and anesthesia time, nurse notes, and indications—everything that explains what you did and why,” Dr. Marks advised. “If you have done a good job in your operative report, it should clearly state the indications for the procedure, the medical necessity for the procedure, and exactly what was done during surgery that corresponds to the codes submitted.”
Conclusion
Several commonly performed procedures are not well described by current CPT codes. As a result, obtaining fair reimbursement requires special attention before and after such procedures. Surgeons should resist the temptation to use CPT codes that are similar to procedures performed when an unlisted code is more appropriate.
Practices should be aware that payers are frequently resistant to preauthorizing the use of unlisted codes, so they should supply information liberally to payers, explaining the nature and necessity for unlisted procedures. Patients must be made aware of existence of unlisted codes and the potential financial implications. Providing patients with information and documenting it are important. It is a good practice to provide flexible payment options for patients who are unable to pay out-of-pocket costs in one lump sum. As with all claim submissions, good documentation in operative notes will be helpful in any cases that require adjudication.
Cheryl Toth, MBA, is director of content development at KZA. The firm partners with AAOS to deliver annual regional coding workshops.