In a study of timing from knee arthroscopy to total knee arthroplasty (TKA), researchers found a relationship between surgery timing and risk of postoperative complications.
Safa C. Fassihi, MD, who presented the findings yesterday, is an adult reconstruction fellow at New York University Langone Orthopedic Hospital.
“In recent years, there has been ample research performed on modifiable risk factors that can be optimized prior to TKA to mitigate postoperative complications,” Dr. Fassihi told AAOS Now Daily Edition.
Several studies have looked at the effect of preoperative corticosteroid or hyaluronic acid injections on subsequent revision risk for TKA, he added. “However, research on the effect of knee arthroscopy timing on subsequent TKA is sparse. While this topic has been examined previously, the time points chosen were typically arbitrary.”
The investigators analyzed insurance data between 2006 and 2017 for patients who underwent TKA with or without previous knee arthroscopy. Of the 132,889 patients included, 5.1 percent (n = 8,863) underwent knee arthroscopy in the two years prior to TKA. The arthroscopy subgroup was further stratified by timing between arthroscopy and TKA: under three months, three to six months, six to nine months, nine to 12 months, and 12–24 months. The team conducted univariate and multivariate analyses to assess relationships between these intervals and TKA outcomes.
“We took a novel approach by utilizing a stratum-specific likelihood ratio (SSLR) analysis, which provides a more data-driven approach for establishing time points at which the risk of revision significantly changes,” Dr. Fassihi said.
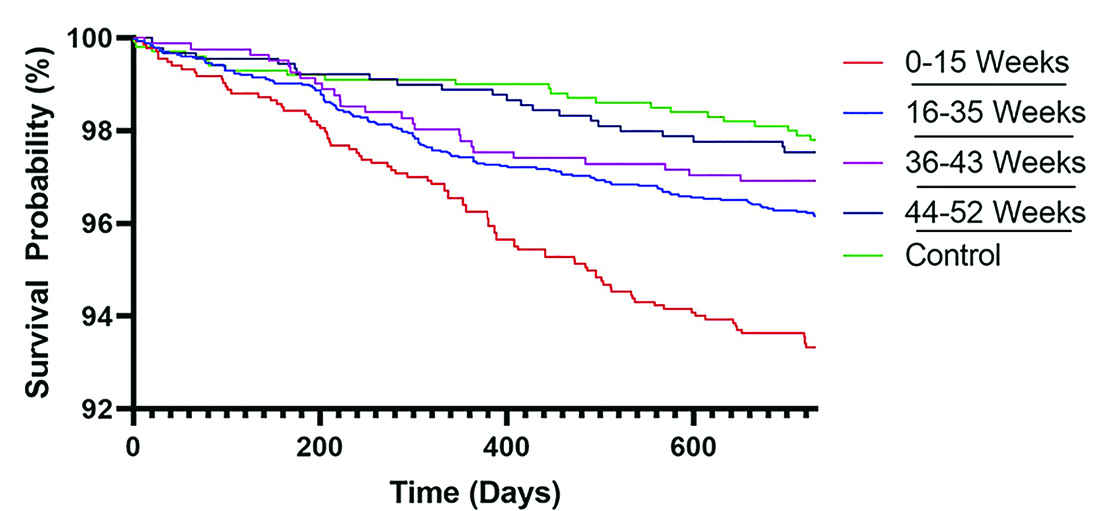
The authors observed an overall trend toward higher risk of complications for patients who underwent TKA within nine months of arthroscopy. The likelihood of revision surgery also was higher among patients with less than three months, three to six months, and six to nine months between procedures (Fig. 1; all P <0.001).
Risk of periprosthetic joint infection (PJI) was also higher in patients who underwent TKA within nine months of arthroscopy (P <0.001). The study authors noted that the association between PJI risk and timing grew stronger as the time between procedures decreased during the nine-month interval.
The clinical takeaway of this study, according to Dr. Fassihi, is that “patients who had less than 35 weeks between knee arthroscopy and subsequent TKA were at increased risk for revision and PJI within two years of TKA. This effect was time-dependent, and, as the time interval between knee arthroscopy and TKA decreased, the risk for subsequent TKA revision and PJI increased.”
The researchers said they were surprised to find that prior arthroscopy increased the risk of surgery after TKA. “The rates of manipulation under anesthesia were significantly increased across all patient cohorts with prior knee arthroscopy—even those who underwent arthroscopy one year before TKA,” said Dr. Fassihi. “We expected this effect in patients with very recent knee arthroscopy but didn’t expect this effect to persist for up to one year.”
The frequency of TKA shortly after initial arthroscopy was also a point of interest for the research team. More than 20 percent of patients underwent TKA within 15 weeks of initial arthroscopy, Dr. Fassihi noted. He hopes the findings of this study “discourage such practice, as the revision risk was markedly higher in these patients.”
Further research is needed to understand the mechanisms behind the relationship between previous arthroscopy and post-TKA PJI.
“Is it caused by the introduction of a low bacterial inoculum into the knee through arthroscopic surgery? Is it caused by scar tissue formation and subsequent wound-healing difficulties? Basic science research may be better able to unearth whether this phenomenon is due to contamination or mechanical factors,” Dr. Fassihi said.
The inability to identify the reasons for arthroscopic intervention represents a limitation of this analysis. This study also was limited by the nature of the large database used and reliance on accurate coding, which is intended for billing rather than research purposes, noted Dr. Fassihi.
“If institutional database research were to reach similar conclusions, it would augment our findings,” he said.
Dr. Fassihi’s coauthors of “Previous Knee Arthroscopy Timing Affects Revision Risk following Total Knee Arthroplasty” are Alex Gu, MD; Lauren E. Wessel, MD; Michael P. Ast, MD; Peter K. Sculco, MD; and Ryan M. Nunley, MD.
Rebecca Araujo is the associate editor of AAOS Now. She can be reached at raraujo@aaos.org.