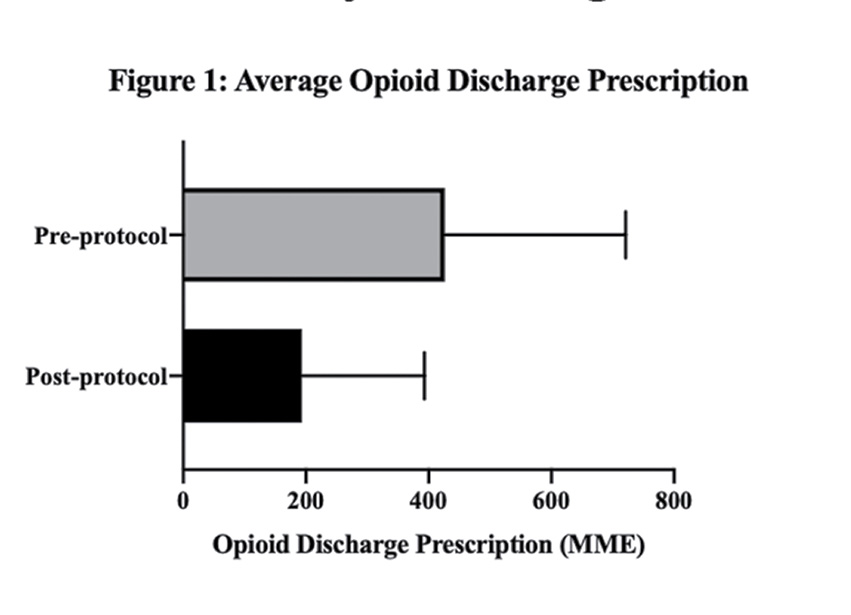
MME = milligram morphine equivalents
In an analysis of an institution-wide reduction of opioid prescribing for patients who have undergone total shoulder arthroplasty (TSA), reductions did not negatively impact patient satisfaction with pain management. The results of the study are reported in a poster on display today in Academy Hall, Sails Pavilion.
As measures to limit the availability of opioids by law and institutional policy become more numerous, the impact of these reductions on patient outcomes, particularly in orthopaedic surgery, has drawn interest.
“We decided to investigate the link between patient satisfaction scores and opioid prescribing for two primary reasons,” presenting author David Bloom, MD, of NYU Langone Health, told AAOS Now Daily Edition. “First, the United States is in the midst of a historic opioid epidemic, and orthopaedic surgeons frequently prescribe these medications. Second, increasing patient satisfaction is a major focus of hospital quality-improvement efforts, so being able to demonstrate that postoperative patient satisfaction is not linked to patient opioid prescription is clinically significant.”
For this retrospective analysis, the researchers assessed 201 patients who underwent TSA between 2014 and 2019, comprising 91 anatomic TSAs and 110 reverse TSAs. Eligible patients had no previous TSA or history of trauma, fracture, or connective tissue disease. The cohort was a combination of inpatients and outpatients, and most patients (>90 percent) were opioid-naïve, Dr. Bloom commented. All participants completed Press Ganey patient satisfaction surveys. In October 2018, study site NYU Langone Health implemented an opioid-reduction protocol. Patients in the analysis were stratified into pre- or post-protocol implementation groups according to surgery date.
In the pre-protocol group, average opioid prescription on discharge was 426.3 ± 295 milligram morphine equivalents (MME), equal to 56.8 tablets of oxycodone 5 mg. After protocol implementation, average prescription at discharge was 193.8 ± 199 MME, equivalent to 25.8 tablets (Fig. 1). Despite the reduction in prescriptions, there was no significant change in satisfaction with pain control, measured via Press Ganey survey (pre-protocol, 4.71; post-protocol, 4.74; P = 0.82). See Table 1 for details about pre- and post-protocol Press Ganey scores.
“The primary finding of this study was that, when postoperative opioid prescribing was reduced, patient satisfaction remained unchanged,” Dr. Bloom said. “Physicians may prescribe fewer opioids following TSA and rest assured that patient satisfaction, as measured by the Press Ganey survey, will likely remain the same provided that there is adequate pain control with nonopioid medications.”
He noted that further analysis is needed to optimize postoperative opioid prescription pill volumes with greater consciousness of relative MME amounts in different opioid options and to eventually aim for “opioid-free” TSA.
The study is limited by its retrospective nature. Use of the Press Ganey survey, to which only a small subset of patients is given the opportunity to respond, is another limitation and “may have exerted a degree of response bias on the results,” added Dr. Bloom.
This study will be presented in poster P0267 on display today in Academy Hall, Sails Pavilion.
Dr. Bloom’s coauthors of “Institutional Reductions in Opioid Prescribing Do Not Change Patient Satisfaction on Press Ganey Surveys after Total Shoulder Arthroplasty” are Amit K. Manjunath, MD; Matthew Gotlin, MD; Eoghan Hurley, PhD; Laith M. Jazrawi, MD; Mandeep Virk, MD; and Young W. Kwon, MD, PhD.
Rebecca Araujo is the associate editor of AAOS Now. She can be reached at raraujo@aaos.org.
