Patients with iron deficiency anemia (IDA) had significantly more complications and greater healthcare utilization after primary total shoulder arthroplasty (TSA) compared to patients without anemia, according to a poster study on display today.
“Anemia is a common health condition that affects 25 percent of the world population and roughly 20 to 35 percent of patients undergoing an elective joint replacement,” presenting author Teja Polisetty, BS, of Harvard Medical School, told AAOS Now Daily Edition. “Recent studies suggest that IDA affects bone metabolism and immunity from infections and can be an independent risk factor for increased morbidity in surgeries with considerable blood loss.”
This retrospective analysis included patients undergoing TSA between 2005 and 2014, identified from a nationwide administrative claims registry. In total, 17,689 patients with IDA were compared with 88,445 matched controls. The two groups were comparable in terms of age, gender, and comorbidities (P = 0.99). The primary outcome was between-group differences in in-hospital length of stay (LOS), medical and implant-related complications, and 90-day episode-of-care costs.
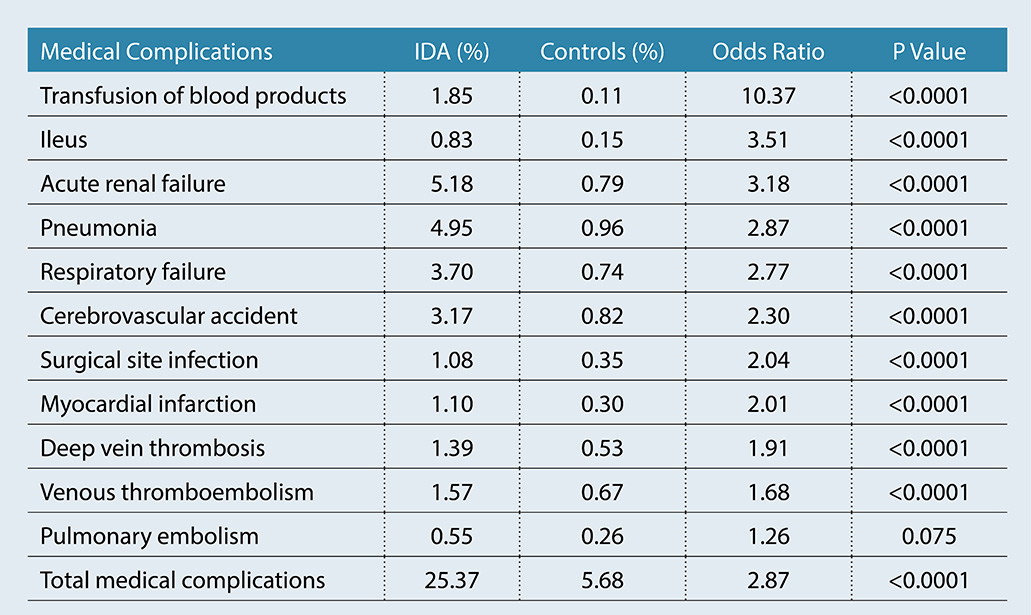
Patients with IDA undergoing TSA had significantly higher incidence of 90-day medical complications compared to matched controls (25.4 percent versus 5.7 percent). IDA was associated with overall greater risk of medical complications, including an increased risk of blood transfusion (all P <0.0001). risk of 90-day implant-related complications was also higher for patients with anemia, including periprosthetic joint infection (all>P <0.0001). see table 1 for full details about 90-day rates of medical complications.>
Mr. Polisetty noted that IDA was also associated with increased incidence and risk of the following complications:
- postoperative periprosthetic fracture (P <0.0001)>
- mechanical loosening (P <0.0001)>
- prosthetic joint dislocation
(P <0.0001)>
Presence of anemia significantly lengthened in-hospital LOS compared to matched controls, at three days versus two days, respectively (P <0.0001). anemia also appeared to increase 90-day episode-of-care costs, which were $14,661 and $13,062 for patients with and without ida, respectively (>P <0.0001).>
“Patients with IDA undergoing primary TSA have significantly longer in-hospital LOS, medical and implant-related complications, and costs of care,” Mr. Polisetty summarized. “Patients at high risk for IDA should be screened regularly to facilitate earlier medical management or specialty referral. Results from this study can be used to counsel professionals and patients with IDA about expected results following TSA as well.”
The authors noted that this study was limited by a lack of stratification by IDA severity, due to the nature of ICD-9 code criteria. In addition, several potential confounding factors could not be assessed due to limitations of the database software and the fact that the ICD-9 data tend to be less granular than clinical follow-up studies.
“Future studies should stratify IDA by the severity and duration of the condition, as this could potentially impact results,” Mr. Polisetty noted.
This study will be presented in poster P0271 on display today in Academy Hall, Sails Pavilion.
Mr. Polisetty’s coauthors of “Iron Deficiency Anemia Is Associated with Increased Medical and Implant-related Complications, Length of Stay, and Costs for Patients Undergoing Total Shoulder Arthroplasty” are Rushabh Vakharia, MD; Andrew Ardeljan, BS; Gagan Grewal, MD; Ajit Vakharia, MD; and Jonathan Chad Levy, MD.
Rebecca Araujo is the associate editor of AAOS Now.