A study presented at the AAOS 2024 Annual Meeting found that application of antibiotic powder to wounds of patients with lower-extremity open fractures demonstrated efficacy in reducing the incidence of deep surgical site infections (DSSIs).
The study, presented by Mir Ibrahim Sajid, MD, of the Orthopaedic Trauma Service at Florida Orthopaedic Institute, involved 261 patients aged 18 years or older with Gustilo-Anderson type III open fractures of the lower extremity treated at four level 1 trauma centers over a span of 3 years. The intervention cohort (A) included 124 (47.5 percent) patients who received antibiotic powder (1 g of vancomycin and 1.2 g of tobramycin) applied directly to the open fracture wound; those patients were compared with a matched historical cohort (B) of 137 (52.5 percent) patients who received identical standard-of-care management except for the antibiotic powder.
The primary outcome was development of DSSI within 6 months, which was defined as a return to the OR for debridement and irrigation and treatment with subsequent culture-specific antibiotics. Secondary post-treatment outcomes included:
- superficial surgical site infection, defined as superficial tissue infection treated with oral antibiotics
- nonunion, defined as fewer than three bridging cortices on orthogonal radiographs at final follow-up at >6 months or hardware failure with no evidence of union at 3 months
- acute kidney injury, defined as an increase in serum creatinine by ≥0.3 mg/dL or formal diagnosis by a medical professional within 48 hours of the study intervention
- deep vein thrombosis or pulmonary embolism
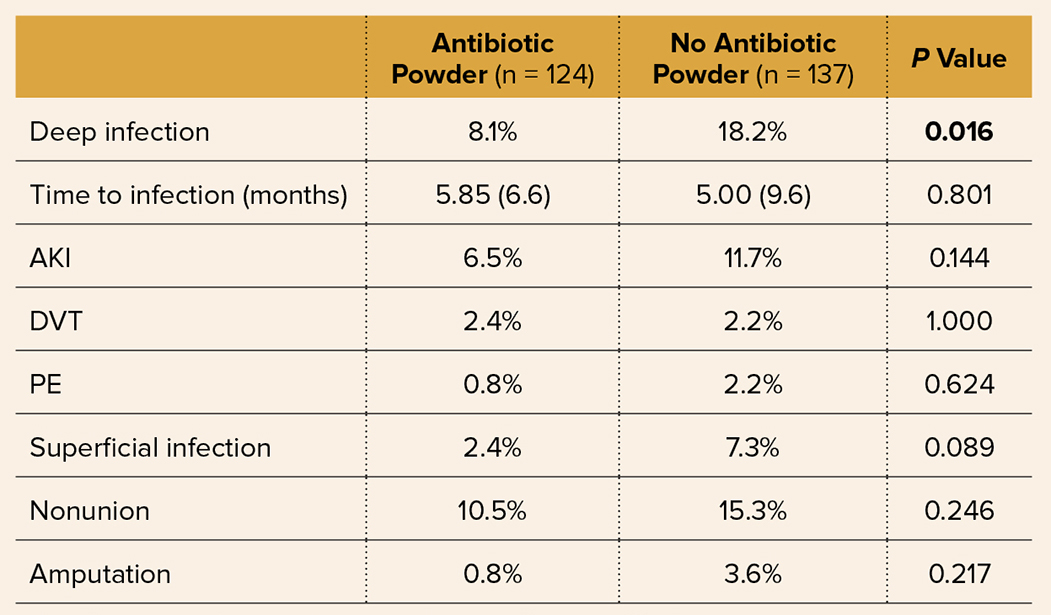
In the powder group, the DSSI rate was 8.1 percent (10/124) compared with 18.2 percent (25/137) in the non-powder group (P = 0.016) at an endpoint of 6 months postoperatively from definitive fixation (Table 1). There were three and 10 superficial surgical site infections in the A and B groups, respectively (P = 0.089).
Overall, the average time to presentation of DSSI was 5.9 months in the A cohort and 5 months in the B cohort. Additionally, patients in the antibiotic powder cohort had lower incidences of superficial infection (2.4 percent versus 7.3 percent), nonunion (10.5 percent versus 15.3 percent), and amputation (0.8 percent versus 3.6 percent). Multivariate regression analysis demonstrated that patients who received antibiotic powder were 65.2 percent less likely to develop DSSI (P = 0.010).
When comparing patient demographics and injury characteristics between the powder and non-powder groups, tobacco use was significantly more prevalent in the powder group (P = 0.005), and immunocompromised status was significantly more prevalent in the non-powder group (P = 0.038). Analysis of patient demographics and injury characteristics demonstrated an association between higher BMI and an increased risk of DSSI (P = 0.029). Analysis did not identify any other demographic or injury characteristics that were associated with increased risk of DSSI, including Injury Severity Score, IIA versus IIIB or IIIC fracture types, or tobacco use.
Dr. Sajid commented that there had been no previous multicenter studies exploring the efficacy of antibiotic powder in reducing the rate of DSSI in type III fractures, which carry a high risk for infection. “Regular [emergency department] protocol for open fractures includes removal of obvious debris, irrigation with normal saline, IV antibiotics, and debridement and irrigation. However, there still has persisted a large percentage of patients who develop DSSI. In an attempt to reduce this rate in a cost-effective way, the idea of antibiotic powder was introduced, and we sought to study its efficacy—which had not been done.”
In terms of the formulation used, the authors observed, “Combining tobramycin with vancomycin is essential for treating Staphylococcal infections—one of the primary organisms for surgical site infection.” In regard to timing, they noted that in their study, antibiotic powder was applied to open type III fractures at the time of presentation to the emergency department, which demonstrated a reduction in DSSI, “suggesting an early intervention to be favorable for open fractures.”
Dr. Sajid noted that another noteworthy finding was the association of BMI with DSSI. “Our study showed that for every unit increase in BMI, the likelihood of developing DSSI increased by 6.7 percent (P = 0.003).”
He said that further large-scale studies are warranted to explore the efficacy, safety, and long-term implications of his study’s findings. Limitations of the study include degree of standardization. “Although institutional protocols were in place to guide management for both the historic and trial cohorts, there are inevitable deviations from the standard, including time to IV antibiotics initiation, exact method of powder application, variability in surgical technique, and time to definitive management,” Dr. Sajid said.
Paper 022 was presented on Monday.
Dr. Sajid’s coauthors of “Assessing the Efficacy of Topical Antibiotic Powder Administration in the Emergency Department on Reducing Deep Surgical Site Infection in Type III Lower Extremity Fractures” are Whisper Grayson, MS; Mitchell John, MD; Bradley J. Lauck; Zohair Zaidi, MD; Alex Savage, MD; Nicole Griffin, MS; Mohamed Awad, MD, MBA; Andrew T. Chen, MD, MPH; John Hwang, MD; Nicholas Alfonso, MD; and Hassan R. Mir, MD, MBA.
Terry Stanton is the former senior medical writer for AAOS Now.