A study found that the adoption and application of patient-reported outcome measures (PROMs) by foot and ankle surgeons may not improve patient experience or activation and may, in fact, decrease understanding or patient activation in select populations.
David N. Bernstein, MD, MBA, MA, a third-year resident in the Harvard Combined Orthopaedic Residency Program, presented the findings in a poster at the AAOS 2023 Annual Meeting. He noted that although PROMs continue to gain popularity in orthopaedic surgery—including among foot and ankle surgeons—the relationship of PROMs and patient activation and patient satisfaction/experience is not well documented. He said he undertook the randomized, controlled trial to address “this previously understudied area of inquiry.”
The study had three objectives:
- To determine whether the active use and discussion of PROMs during new patient visits are associated with patient satisfaction and experience.
- To determine whether the active use and discussion of PROMs during new patient clinic visits are associated with patient activation.
- To determine whether objectives (1) and (2) differ based on surgeon or sociodemographic factors.
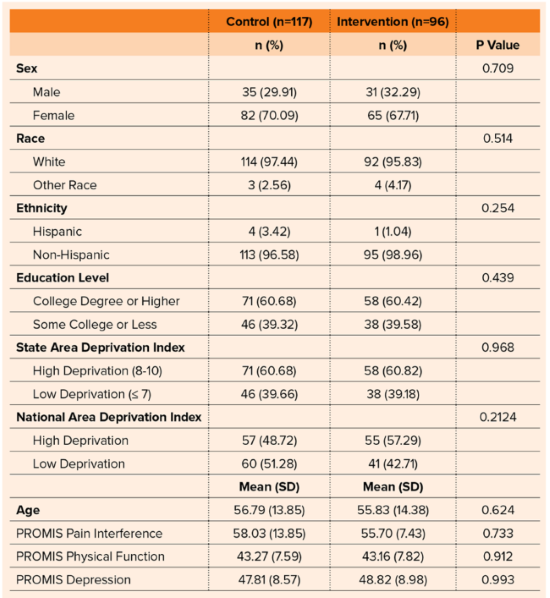
The study group included 213 patients who presented to a foot and ankle clinic at a single academic medical center over a period of 13.5 months. After randomization, 117 were in the control group and 96 were in the intervention cohort. The intervention cohort was able to view and discuss their PROM results with their physicians.
No difference was seen in baseline patient characteristics between the two groups. The researchers used the Consumer Assessment of Healthcare Providers and Systems Clinician and Group Survey (CG-CAHPS) to assess satisfaction. Across the four survey questions, there was no difference in satisfaction between patients in the intervention versus control groups (P >0.05) (Table 1).
There was no difference in scores on the Patient Activation Measure (PAM), a 10– or 13-item survey that assesses an individual’s knowledge, skills, and confidence integral to managing one’s own health and healthcare, between the two groups (intervention, 70.99 [SD = 15.35] versus control, 72.38 [SD: 14.84], P = 0.50).
There continued to be no difference in PAM scores between the two groups when clustered by surgeon (P >0.05). Among patients whose Area Deprivation Index (ADI) national percentile was below the 50th percentile, there was a similar percentage of subjects whose PAM scores were either a 3 or 4 between intervention and control subjects (85.37 percent versus 85.00 percent, respectively). However, among patients whose ADI national percentile was above the 50th percentile (i.e., patients with greater disadvantage), intervention subjects were less likely to have a PAM score of 3 or 4 compared to controls (85.45 percent versus 94.7 percent).
Of the findings, the authors wrote: “The pivotal finding in this study suggests the most socially deprived patients in our sample who were randomized to viewing and discussing their PROMs results had lower patient activation. Important to add, this group still assessed their providers highly. In contrast, the group with a lower ADI (i.e., less disadvantaged) appeared to be more engaged by the review of this PROMs information at the time of the clinic visit. This may reflect the need for altered presentations of the data or specific training for health literacy or communication to better activate different patient groups.”
Dr. Bernstein commented, “We know PROMs can play an important role in providing optimal patient care, but our results of this study demonstrate there is greater nuance than previously appreciated.” He said that although PROMs are a core component of patient-centered care, “How we present the results to patients—and to which patients we present—them matters. Further, surgeons who are already highly rated by patients may not benefit as much from explaining PROMs in detail.”
On the study’s limitations, Dr. Bernstein noted that the study involved a single center and specifically patients presenting to the foot and ankle clinic. “While we focused on new patients only, we did not focus on one pathology,” he said. “Also, we were not powered to study all possible interactions, including that between both surgeon and socioeconomic status simultaneously.”
He said the results point to a need for further study of several factors. First, he said, “It remains unknown what the best way is to present PROMs to patients.” Second, “It is unclear exactly what patient populations would benefit the most, including what conditions and among what sociodemographic factors.” Third, “It is unclear if our findings are generalizable outside of foot and ankle surgery.”
Dr. Bernstein noted, “Highly rated foot and ankle surgeons who show and discuss PROMs results may not improve patient experience or activation and may, in fact, decrease understanding or patient activation in select populations.” Thus, he said, “Future work is needed to determine when PROMs discussions are most beneficial and how best to present PROMs data, as we suspect that how the information was presented—and not the use of PROMs—resulted in our findings. Health literacy tools and/or communication training may better engage different patient groups regarding PROMs.”
Dr. Bernstein’s coauthors of “Does Patient-reported Outcome Measure Use at New Foot and Ankle Clinic Visits Improve Patient Satisfaction and Experience? A Randomized, Controlled Trial” are Courtney M. C. Jones, PhD, MPH; A. Samuel Flemister, MD; Benedict F. DiGiovanni, MD; and Judith F. Baumhauer, MD, MPH.
Terry Stanton is the senior medical writer for AAOS Now.