
Hip-spine biomechanics has become an increasingly popular subject of study over the past several years. Approximately 4.5 percent of all total hip arthroplasty (THA) patients have had a prior lumbar spine surgery. The number of lumbar spinal fusion surgeries performed has increased anywhere from 60 percent to 300 percent over the past two decades. Recent research has focused on lumbopelvic kinematics and hip instability, particularly as they pertain to acetabular cup position. Recent studies have demonstrated that prior spinal fusion surgery is correlated with an increased dislocation risk as well as poorer functional outcome scores after THA. History of lumbar spinal fusion surgery has been shown to be a stronger predictor of hip instability than both Parkinson’s disease and dementia. This has translated into an increased relative risk of revision surgery in THA patients with spinal disease. This article serves as a brief review of hip-spine biomechanics and its clinical implications in patients undergoing THA.
Pelvic sagittal plane kinematics (particularly reduced pelvic mobility) play a key role in hip instability after THA. In a 2016 Mayo Clinic cohort study of 9,784 patients, 58 percent of THA dislocations had an acetabular component position within the Lewinnek “safe zone.” This finding suggests that extrinsic factors, such as varying hip-spine biomechanics, may be contributing to the complex issue of hip instability. For patients with lumbar spine pathology, the ideal cup position may even lie outside the previously established safe zone. A closer look at sagittal plane kinematics in patients with reduced spinopelvic motion has provided insights that may ultimately decrease revision rates in this subset of patients.

Spinopelvic motion is calculated with several sagittal plane angles in both the sitting and standing positions. When moving from a seated to standing position, the pelvis tilts anteriorly with the lumbar spine in lordosis. This creates a balanced trunk with the acetabulum over the femoral head. When sitting, the pelvis tilts posteriorly as the spine loses its lordosis. This increase in anteversion and inclination is known as the biological opening of the acetabulum to accommodate the femoral head in the seated position. Termed the ante-inclination or sagittal acetabular angle, this value can be measured on a lateral spine-pelvis radiograph with a normal reported value between 41 degrees and 63 degrees.
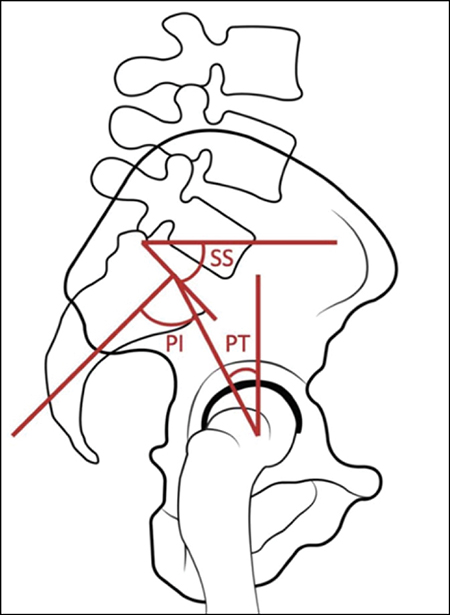
Lateral spine-pelvis radiographs are also useful in calculating sacral slope (SS) and, more specifically, change in slope between seated and standing positions. It is now understood that a change in SS of fewer than 10 degrees between the sitting and standing positions places patients at an increased risk for dislocation. SS has been shown to be the most reproducible measurement in assessing pelvic motion.
Pelvic tilt (PT) is measured as an angle formed by a line from the S1 endplate to the center of the femoral head and a vertical line on the sagittal view. PT is often used to describe the standing tilt of the pelvis. The sum of these two dynamic parameters (SS and PT) equals a constant referred to as pelvic incidence (PI). The behavior of these two functional values determines the ideal cup position in the sagittal plane. PI can be thought of as a fixed measurement of anterior to posterior pelvic dimension and determines the position of the spine relative to the center of the femoral heads, with a normal range of 25 degrees to 85 degrees. Studies have suggested factors influencing PI, including genetics and other heritable aspects of sagittal spine balance (Fig. 1).
Reduced spinopelvic motion is generally defined as fewer than 10 degrees of pelvic motion between seated and standing positions. Degenerative disk disease, spondylosis, ankylosing spondylitis, and spinal fusion are some common reasons for reduced mobility. Different classification systems and types of stiffness have been described—most commonly loss of anterior or posterior pelvis tilt, termed “stuck sitting” and “stuck standing,” respectively.
A patient determined to be stuck standing exhibits loss of posterior PT when sitting and increased risk for anterior impingement and posterior instability. These findings are due to the change in functional anteversion of the acetabulum, as it has been established that for every degree of posterior PT, there is an associated 0.8-degree increase in acetabular anteversion. This allows the femur to flex forward without impinging on the anterior acetabulum during sitting (Fig. 2).
On the contrary, for a patient who is stuck sitting with loss of lumbar lordosis, a relative outlet view is seen on standing anterior-posterior radiographs due to loss of normal anterior PT when standing. This increases the risk of posterior impingement and anterior instability. For example, in elderly patients with degenerative lumbar changes resulting in loss of lordosis, an increased standing posterior PT functionally increases the anteversion and overall ante-inclination of the acetabulum.
An understanding of these parameters has led some authors to advocate for modifying acetabular component position based on spinopelvic alignment and flexibility. The Lewinnek safe zone theory has been demonstrated to be an incomplete guide to acetabular component position, as it is limited by its nature of being a static anterior-posterior image that does not take into account these critical spinopelvic parameters.
Although the appreciation of hip and spine biomechanics has improved significantly, the clinical application of this knowledge remains unclear. Many studies have advocated for the use of dual-mobility constructs in patients with spinopelvic abnormalities, with good clinical and cost-effective outcomes. However, few studies have investigated the magnitude of the effect that surgical approach for THA has on this at-risk population. As a result, it is thus far unclear whether the published treatment algorithms for acetabular component positioning based on hip-spine pathology should be utilized for all hip approaches.
Huthayfa Kahf, MD, is a fourth-year orthopaedic surgery resident at the University of California, Irvine.
Steven Yang, MD, MBA, FAAOS, is an assistant clinical professor of orthopaedic surgery at the University of California, Irvine, and is the chief of the arthroplasty service.
References
- Bozic KJ, Lau E, Ong K, et al: Risk factors for early revision after primary total hip arthroplasty in Medicare patients. Clin Orthop Relat Res 2014;472(2):449-54.
- Stefl M, Lundergan W, Heckmann N, et al: Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J 2017;99-B(1)(Suppl A):37-45.
- Martin BI, Mirza SK, Spina N, et al: Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine 2019;44(5):369-76.
- Perfetti DC, Schwarzkopf R, Buckland AJ, et al: Prosthetic dislocation and revision after primary total hip arthroplasty in lumbar fusion patients: A propensity score matched-pair analysis. J Arthroplasty 2017;32:1635-40.e1.
- Eneqvist T, Nemes S, Brisby H, et al: Lumbar surgery prior to total hip arthroplasty is associated with worse patient-reported outcomes. Bone Joint J 2017;99-B:759-65.
- Buckland AJ, Puvanesarajah V, Vigdorchik J, et al: Dislocation of a primary total hip arthroplasty is more common in patients with a lumbar spinal fusion. Bone Joint J 2017;99-B:585-91.
- Loh JLM, Jiang L, Chong HC, et al: Effect of spinal fusion surgery on total hip arthroplasty outcomes: a matched comparison study. J Arthroplasty 2017;32:2457-61.
- Abdel MP, von Roth P, Jennings MT, et al: What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin Orthop Relat Res 2016;474(2):386-91.
- Lazennec JY, Charlot N, Gorin M, et al: Hip-spine relationship: a radio-anatomical study for optimization in acetabular cup positioning. Surg Radiol Anat 2004;26(2):136-44.
- Sadhu A, Nam D, Coobs BR, et al: Acetabular component position and the risk of dislocation following primary and revision total hip arthroplasty: a matched cohort analysis. J Arthroplasty 2017;32(3):987-91.
- Brown TD, Elkins JM, Pedersen DR, et al: Impingement and dislocation in total hip arthroplasty: mechanisms and consequences. Iowa Orthop J 2014;34:1-15.
- Frandsen JJ, Kahn TL, Anderson LA, et al: Managing hip-spine concepts in the direct anterior approach with use of fluoroscopy. J Arthroplasty 2021;36(7S):S104-10.
- Luthringer TA, Vigdorchik JM: A preoperative workup of a “hip-spine” total hip arthroplasty patient: a simplified approach to a complex problem. J Arthroplasty 2019;34(7S):S57-70.
- Turgeon TR, Hedden DR, Bohm ER, et al: Radiostereometric analysis and clinical outcomes of a novel reverse total hip system at two years. Bone Jt Open 2023;4(5):385-92.