
Originally developed as research tools to better elucidate pathological gait deviations, the tools and techniques associated with quantitative gait analysis have expanded rapidly and are now more accessible than ever as clinical resources. Over the past decade, the increased accessibility of these tools has allowed clinicians to identify new indications for their use, including increasing applications to orthopaedic care and trauma surgery. The purpose of this article is to inform readers of the history and current practice of one of the early adopters of clinical gait analysis, Rancho Los Amigos National Rehabilitation Center’s Pathokinesiology Laboratory. At this specialty referral service, clinicians work closely with referring physicians to ensure that the service continues to be an effective foundational step in treatment and/or surgical planning workflows.
Founded in 1968 by the pioneering orthopaedic surgeon Jacquelin Perry, MD, the Pathokinesiology Lab at Rancho Los Amigos National Rehabilitation Center has a long history of using quantitative approaches to analyze gait and other functional activities. To this day, the lab continues to use methods originally developed by Dr. Perry and other early gait researchers, including fundamental biomechanics principles and quantitative measurements of muscle activity, to guide therapeutic and surgical treatments for patients with movement disorders. Referred patients have a wide range of diagnoses, including cerebral palsy, traumatic brain injury, stroke, peripheral neuropathy, and post-traumatic and degenerative conditions, or they are under consideration for orthopaedic surgical interventions. As a result, clinical questions focused on improving movement outcomes vary among individuals, and testing may include general functional diagnostic tests, data to supplement or substitute for classic static assessments such as CT, or tests to address questions related to the deficiencies of a single muscle. However, the quantitative approach allows the lab to assess each patient’s impairments and functional limitations and piece together an understanding of how neuromuscular deficits influence movement execution.
Based on decades of clinical and research work, the lab has come to recognize that individual muscle dysfunction is a common but often uninvestigated source of movement dysfunction. Examples of typical questions addressed include:
- identifying which muscles/structures are contributing to the patient’s functional limitations
- determining whether a noninvasive therapeutic program would be indicated to optimize the patient’s function, such as orthotic support, assistive devices, or muscle strengthening (via exercise and/or electrical stimulation)
- determining whether a patient would benefit from surgical or pharmacological intervention
- delineating what surgery should be performed
The lab believes that its detailed and data-driven approach maximizes patients’ outcomes and minimizes complications, unsuccessful and/or detrimental surgeries, and the potential need for multiple procedures.
Depending on the patient’s needs, a lab visit may include analyses of muscle activity, joint motion (kinematics), joint forces and moments (kinetics), foot pressure and center of pressure, isometric muscle strength assessment, or energy expenditure. As part of the analysis, data collected from each patient are compared to a large database of information on normal human movement. In order to identify the underlying causes, the lab evaluates any movement deficits in light of clinical measurements of the patient’s muscle weakness, spasticity, joint contracture, or other measurable impairments.
The quantitative methodology truly shines in complex cases where less conservative treatments such as surgical interventions are being considered. For example, what if a patient presents with foot/ankle pain while using an ankle foot orthosis and exhibits excessive inversion throughout the gait cycle during barefooted walking? Is the observed deviation a result of an overactive posterior tibialis? Or is it due to a muscle imbalance? Is it some other neuro-musculoskeletal factor? Ultimately, does the presentation require the surgical procedure being considered (e.g., posterior tibialis lengthening), a different procedure (e.g., split anterior tibial tendon transfer and/or tendo-Achilles lengthening), or maybe just a different conservative approach to address deficits elsewhere in the lower limb? The lab’s combined biomechanics and muscle-activity testing procedures answer these questions, greatly reducing the likelihood of detrimental surgical procedures being performed. Indeed, many patients referred for verification prior to posterior tibialis lengthening end up requiring a completely different procedure and/or additional procedures.
Collecting all the necessary data for these analyses is no small feat, but the data are essential in developing treatment plans for those with complex conditions. Patients typically spend 4 to 6 hours in the lab on the day of testing. Following a review of the patient’s history and a qualitative assessment of muscle strength and joint range of motion, the clinical team works to place all the necessary sensors on the patient. Most patients are instrumented with 4 to 10 fine-wire electrodes to measure muscle activity. Electrodes are inserted directly into the muscles of interest with a small needle. When the needle is removed, the electrodes remain in the muscle and the hair-like wires are connected to an external ground plate and amplifier. Staff then verify electrode position by applying a small electrical impulse into the wire and observing muscle contraction and/or tendon movement.
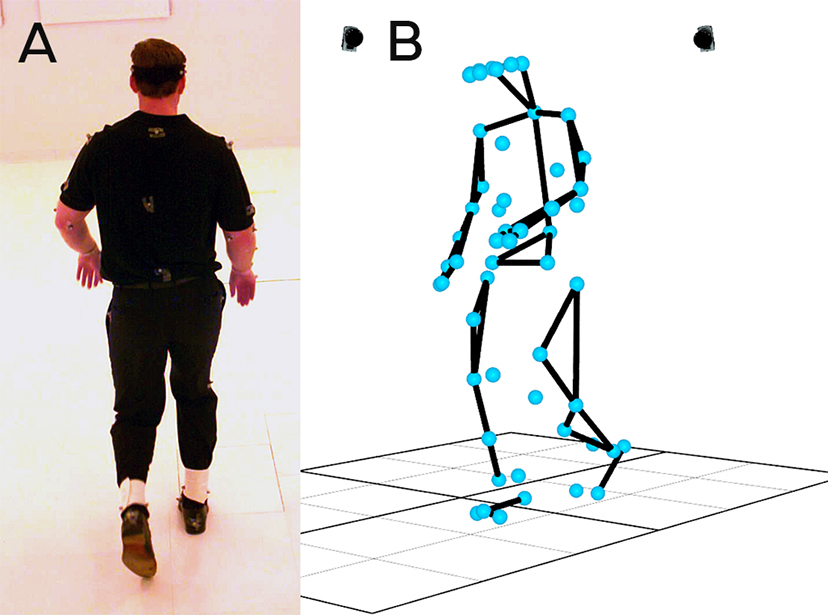
After electrode insertions are complete, multiple reflective markers are placed on various anatomical locations to collect the position and orientation of different body segments (Fig. 1). The number of markers varies based on patient presentation (typically 18 to 45 markers). The markers are designed to reflect the infrared light emitted by cameras and, when the space is calibrated, allow staff to determine the 3D location of each marker throughout the movement. Sensors are also added to the bottom of the patient’s foot/shoe to measure foot-floor contact patterns and center of pressure progression. Once completely instrumented, a patient needing gait analysis is typically asked to walk at free and fast self-selected speeds under various conditions, such as barefoot, shod and/or with orthoses, or while using an upper-extremity ambulatory aide (e.g., single-point cane). Preparation, placement, and verification of the sensors take up most of the patient’s time; the actual collection of data during walking or functional activity may only take 30 minutes to an hour. Then the real work begins after the patient leaves, when the team of biomechanics experts takes the collected data, processes and analyzes the results, and synthesizes a report and treatment recommendations for the referring physician.
Although data collection and analysis require a substantial amount of time and effort, the lab staff finds the work fulfilling, as their understanding of neuromuscular biomechanics greatly improves the quality of life of those they treat. They are truly grateful for the foundation established by Dr. Perry and are proud to honor her innovative and progressive spirit by continuing to conduct high-quality, quantitative movement analysis in a clinical setting.
Quantitative gait analysis can be covered by both private and government medical insurance programs. However, despite increasing clinical accessibility, specialty gait-analysis services can still be difficult to find. If you are interested in specialty gait analysis, reach out to large rehabilitation centers near you that may provide specialty services. If you continue to have difficulty finding a local gait-analysis service, please do not hesitate to contact the Pathokinesiology Laboratory. Out-of-state referrals to the lab are considered on a case-by-case basis, but the lab may be able to guide you toward a service closer to where you practice.
Jeffery W. Rankin, PhD, would like to thank Lisa Haubert, MPT, DPT, KEMG, and Walter Weiss, MPT, NCS, for assistance with preparing this article.
Dr. Rankin has almost two decades of experience in conducting and leading movement biomechanics research spanning sport and clinical rehabilitation settings. He is currently the acting director of the Pathokinesiology Lab and director of the Rehabilitation Engineering Program at Rancho Los Amigos National Rehabilitation Center, where he oversees a specialty outpatient physical rehabilitation service and several federally funded research projects aimed at improving the lives of those with movement disorders.