Editor’s note: The following article is a review of a video available via the AAOS Orthopaedic Video Theater (OVT). AAOS Now routinely reviews OVT Plus videos, which are vetted by topic experts and offer CME. For more information, visit aaos.org/OVT.
Equinocavovarus deformity challenges patients. For ambulatory patients, the dynamic deformity makes wearing shoes and ambulating difficult. For non-ambulatory patients, lack of a plantigrade foot makes transfers more difficult and can lead to lateral skin breakdown. The deformity can be encountered in patients who have an upper motor neuron disorder or injury such as stroke, traumatic brain injury (TBI), or cerebral palsy, as well as clubfoot. Although these patients may often be referred to foot and ankle orthopaedic specialists, any surgeon comfortable with the anatomy can readily address a flexible equinocavovarus deformity.
The OVT Plus video presented by Isaiah Xerxes Hughes, BS; Erik C. Freeland, DO, FAAOS; and Adel Mahjoub, MD, demonstrates a technique for creating a balanced plantigrade foot for a patient with a progressive deformity following TBI using a split anterior tibial tendon (ATT) transfer (SPLATT) with tendo-Achilles lengthening (TAL) and flexor tendon z-lengthening. The patient history notes that appropriate conservative treatment for the deformity, an ankle-foot orthosis, had failed.
A physical exam must confirm a flexible deformity; fixed bony deformity will require osteotomies and/or fusions. Surgical goals should be reviewed with the patient. Depending on the underlying disease and motor function, the procedure may improve active dorsiflexion or eversion or may only provide a check-rein procedure to restore a balanced plantigrade foot and prevent progression of deformity.
For surgical planning, the video includes multiple necessary incisions. Planning and marking all incisions at the start of the procedure ensure adequate skin bridges.
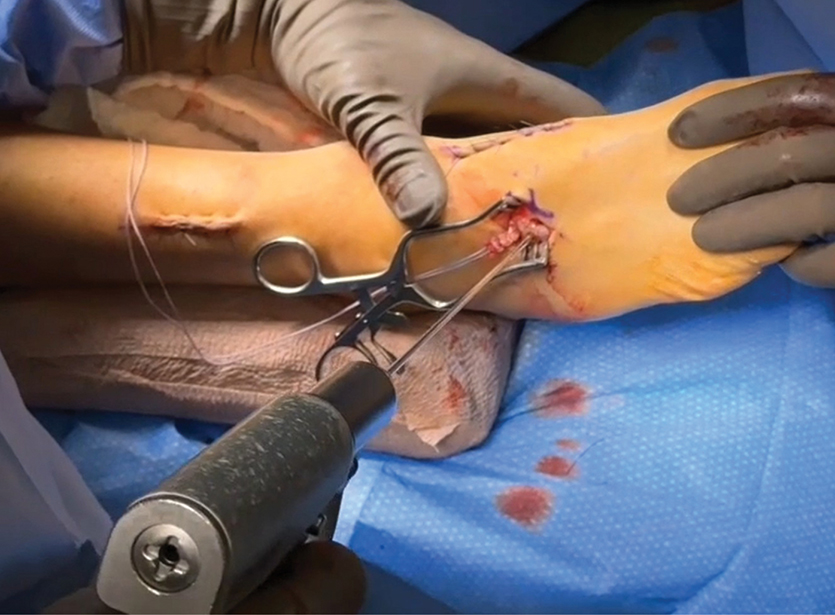
Tendon lengthenings are performed, starting with a percutaneous TAL followed by the posteromedial approach to the posterior tibial tendon, flexor digitorum longus, and flexor hallucis longus. The video notes the importance of long limbs for the z-lengthening (Figure 1). This vital step ensures continued apposition of the proximal and distal tendon portions after retraction occurs following release of the shortened tendon.
In this video, the surgeons did not repair the tendons due to lack of functioning flexor muscles. In many cases, after completion of the SPLATT, the surgeons would return to the lengthened tendons for repair at their new length, often using multiple stitches with a braided, non-resorbable suture of a size appropriate to the tendon diameter.
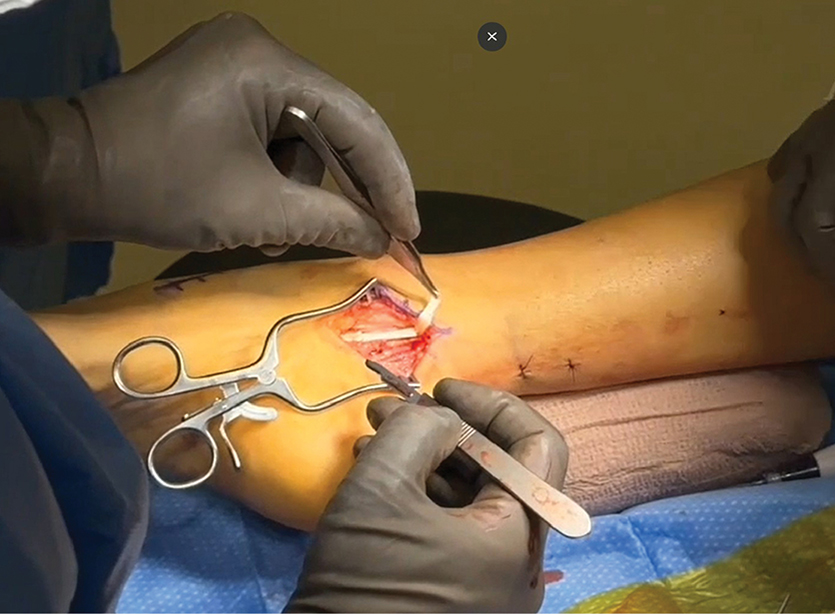
The video next presents ATT transfer to the lateral midfoot. After releasing the most lateral portion of the ATT at its most distal extent, it is identified through a more proximal incision and carefully split with a suture. This split lateral limb is then inserted into the lateral cuneiform using an interference screw technique (Figure 2). The surgeon can choose fixation into either the cuboid or the lateral cuneiform. A recent study by Craft et al. using SPLATT for residual clubfoot found no difference in recurrence rates with either choice.
This video clearly demonstrates an approach to correct a flexible equinocavovarus deformity using orthopaedic fundamentals. For patients with preoperative muscle function, repair of the lengthened flexor tendons is appropriate.
However, even in the absence of active muscle control, this procedure has value to create a plantigrade, braceable foot that is more functional and less prone to skin complications.
Alexandra Page, MD, FAAOS, is a foot and ankle specialist in private practice in San Diego. She is deputy editor of AAOS Now.
References
- Lullo B, Nazareth A, Rethlefsen S, et al. Split tibialis anterior tendon transfer to the peroneus brevis or tertius for the treatment of varus foot deformities in children with static encephalopathy: A retrospective case series. J Am Acad Orthop Surg Glob Res Rev. 2020;4(5):e2000044. doi:10.5435/JAAOSGlobal-D-20-00044
- Craft M, Calhoon G, Lewis TR. Tibialis anterior tendon transfer for clubfoot deformity: Cuboid versus lateral cuneiform. J Pediatr Orthop. 2025;45(3):164-168. doi:10.1097/BPO.0000000000002852
Video details
Title: Bilateral Split Anterior Tibial Tendon Transfer and Flexor Tendon Lengthening
Authors: Isaiah Xerxes Hughes, BS; Erik C. Freeland, DO, FAAOS; Adel Mahjoub, MD
Published: 2025
Time: 7:35
Tags: Foot and ankle, Surgical exposure, Tendons
Visit aaos.org/OVT to view this award-winning title and more than 1,600 other videos from across orthopaedic topics, institutions, practice management, and industry.