When the wars in Iraq and Afghanistan surged, so did the complexity and severity of injuries sustained by U.S. service members. Military surgeons were confronted with new challenges — massive extremity wounds from blasts, complex open fractures, limb-threatening vascular injuries, and devastating infections — many of which had no precedent in civilian trauma literature. It quickly became apparent that treating these injuries would require not only innovative clinical strategies but also a dedicated research enterprise, unlike anything the military had developed to that point.
By 2007, more than 80% of battlefield injuries in U.S. military personnel involved extremities. The vast majority were high-energy, open injuries that often required staged reconstruction, lengthy rehabilitation, and complex decisions about amputation versus limb salvage. These injuries also carried high risks of chronic pain, disability, and secondary complications such as infection, post-traumatic arthritis, and heterotopic ossification. Unfortunately, the military alone lacked the patient volume and research infrastructure needed to study these rare but devastating injuries in a rigorous, prospective fashion. Most available evidence at the time was limited to small case series or retrospective reviews.
Even as military surgeons gained unparalleled experience treating combat trauma, they knew that many of the answers they needed would only come from leveraging the volume and academic capabilities of the civilian trauma network. One such collaboration is the Major Extremity Trauma Research Consortium (METRC), a research network with the mission of conducting large-scale, prospective, multicenter trials focused on the most pressing clinical questions in combat and civilian extremity trauma.
In 2006, AAOS, in collaboration with the Orthopaedic Trauma Association and the Society of Military Orthopaedic Surgeons, convened the first Extremity War Injuries (EWI) symposium. These annual meetings, now in their second decade, are a vital forum for identifying gaps in combat casualty care and aligning military and civilian research priorities.
Advocacy efforts stemming from EWI have historically proven highly effective. In 2008 and 2009, Congress responded by appropriating more than $100 million in new peer-reviewed research funding for extremity war-injury research. This was a landmark win for orthopaedic trauma patients — before 2006, no federal dollars had been dedicated to this type of orthopaedic trauma research.
Out of this momentum, METRC was born in 2009. Funded initially by the Department of Defense (DOD), METRC brought together four military treatment facilities and 20 civilian level I trauma centers into a single, coordinated research network.
This collaborative model has since produced a growing portfolio of impactful clinical research. METRC is now a collaboration of 90 centers, enrolling more than 24,000 patients in 35 multicenter studies, publishing more than 90 impactful peer-reviewed manuscripts, and attracting more than $150 million in competitive grant funding from the DOD, Patient-Centered Outcomes Research Institute (PCORI), and the National Institutes of Health. In 2023, AAOS recognized METRC’s contributions with the prestigious Elizabeth Winston Lanier Kappa Delta Award for its extraordinary impact on orthopaedic trauma research.
Translating research into clinical practice
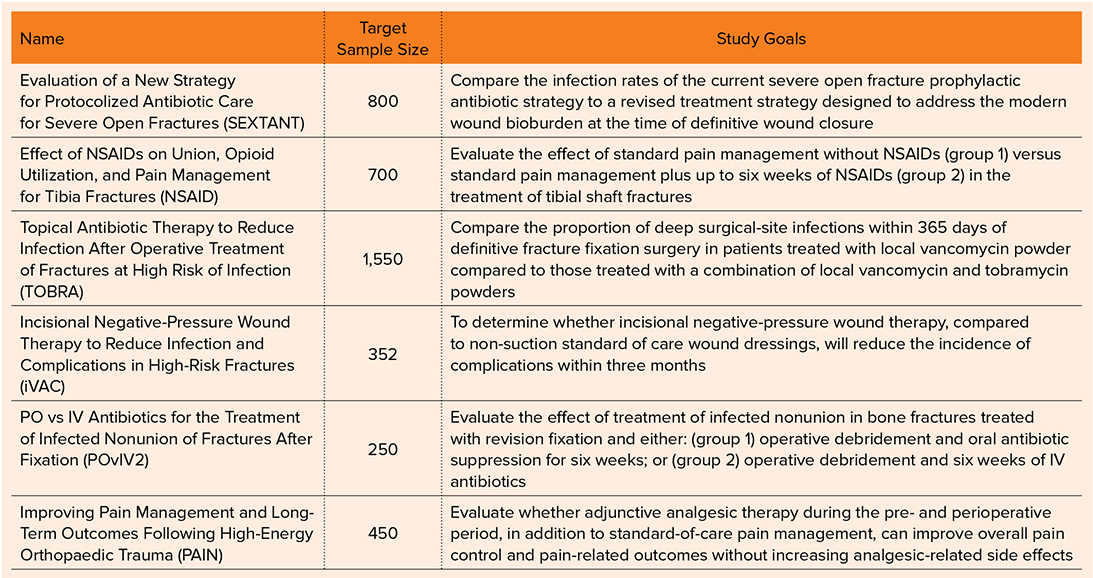
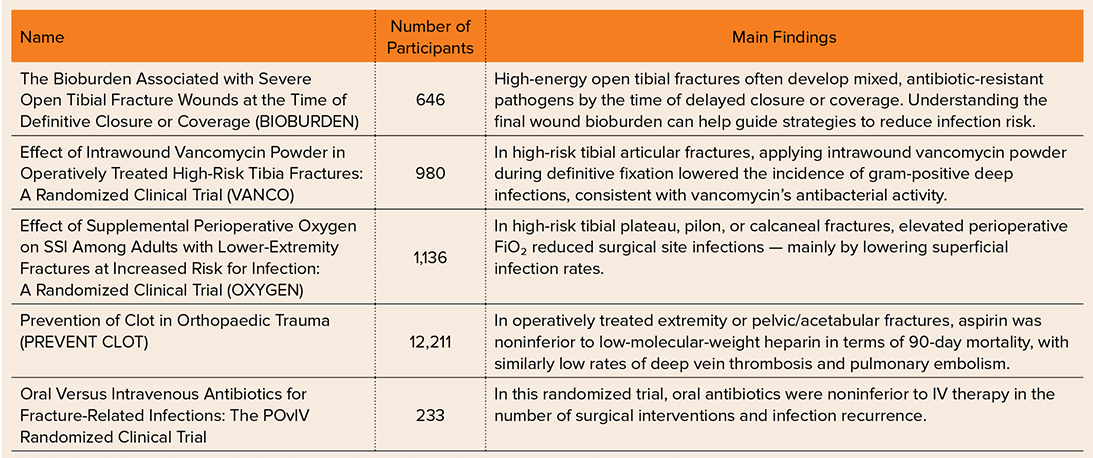
Ultimately, METRC will be judged by its impact on clinical care. Through METRC, orthopaedic trauma surgeons have tackled complex clinical questions of interest to military and civilian populations that were once thought nearly impossible to study in trauma populations. METRC studies are typically large, randomized, multicenter trials with rigorous study designs that increase the chances of influencing clinical practice. Table 1 summarizes the completed trials from METRC, along with key findings; Table 2 lists ongoing studies and their goals.
The METRC investigations — exploring topics such as compartment syndrome and best fixation strategies for mangled limbs — reflect the power of a coordinated, multicenter approach to improve care for orthopaedic trauma patients.
Securing the future
As the memory of recent wars fades, so does the urgency behind sustained research funding. But the need to advance the field has not gone away. Thousands of veterans continue to live with the sequelae of blast injuries, and the next conflict may be just over the horizon. Simultaneously, high-energy civilian trauma — from motor vehicle crashes to mass casualty events — remains all too common, with much work left to do to improve the often devastating consequences.
The orthopaedic community must not lose the momentum gained over the past 15 years. Continued funding through the DOD’s Peer Reviewed Orthopaedic Research Program and strategic support for METRC and the EWI symposia are essential to maintaining readiness and improving care for all trauma patients.
Despite the track record of success, recent funding through the DOD Congressionally Directed Medical Research Program earmarked for orthopaedic trauma was reduced from $30 million per year to $0 in the most recent funding cycle. However, there is hope that the improved orthopaedic care resulting from METRC investigations will prove the worth of civilian-military partnerships, ultimately leading to restored funding for this critical work.
Born on the battlefield and now felt in trauma centers around the nation, the story of METRC is a testament to the power of partnership — military and civilian surgeons working side by side, united by a shared goal to improve outcomes after devastating injuries. The future of the field depends on this collaboration. By continuing to invest in the infrastructure and scientific rigor of these collaborative efforts, we can ensure that the sacrifices made in the past fuel more effective care for the injured — no matter where or how they serve.
Army Col. Daniel J. Stinner, MD, PhD, is an active-duty Army orthopaedic trauma surgeon and professor of orthopaedic surgery at Vanderbilt University Medical Center.
Robert V. O’Toole, MD, is the Hansjörg Wyss Medical Foundation Endowed Professor in Orthopaedic Trauma at the University of Maryland R Adams Cowley Schock Trauma Center, where he serves as division head of orthopaedic traumatology.
Katherine P. Frey, PhD, MPH, RN, is an associate scientist at the Johns Hopkins Bloomberg School of Public Health in the Department of Health Policy and Management and associate director of METRC.
References
- Stinner DJ, Wenke JC, Ficke JR, et al. Military and civilian collaboration: The power of numbers. Mil Med. 2017;182(S1):10-17. doi:10.7205/MILMED-D-16-00138
- Major Extremity Trauma Research Consortium. Building a clinical research network in trauma orthopaedics: The Major Extremity Trauma Research Consortium (METRC). J Orthop Trauma. 2016;30(7):353-361. doi:10.1097/BOT.0000000000000549
- The Major Extremity Trauma Research Consortium. The Major Extremity Trauma Research Consortium: Development and impact of an orthopaedic trauma research program. J Am Acad Orthop Surg. 2023;31(18):945-956. doi:10.5435/JAAOS-D-23-00311
- Major Extremity Trauma Research Consortium. The bioburden associated with severe open tibial fracture wounds at the time of definitive closure or coverage: The BIOBURDEN Study. J Bone Joint Surg Am. 2024;106(10):858-868. doi:10.2106/JBJS.23.00157
- Major Extremity Trauma Research Consortium, O’Toole RV, Joshi M, et al. Effect of intrawound vancomycin powder in operatively treated high-risk tibia fractures: A randomized clinical trial. JAMA Surg. 2021;156(5):e207259. doi:10.1001/jamasurg.2020.7259
- Patterson JT, Slobogean GP, Gary JL, et al. The VANCO trial findings are generalizable to a North American trauma registry. J Orthop Trauma. 2024;38(1):10-17. doi:10.1097/BOT.0000000000002704
- Goldman AH, Tetsworth K. AAOS Clinical Practice Guideline summary: Prevention of surgical site infection after major extremity trauma. J Am Acad Orthop Surg. 2023;31(1):e1-e8. doi:10.5435/JAAOS-D-22-00792
- Major Extremity Trauma Research Consortium. Effect of supplemental perioperative oxygen on SSI among adults with lower-extremity fractures at increased risk for infection: A randomized clinical trial. J Bone Joint Surg Am. 2022;104(14):1236-1243. doi:10.2106/JBJS.21.01317
- Major Extremity Trauma Research Consortium, Obremskey WT, O’Toole RV, et al. Oral vs intravenous antibiotics for fracture-related infections: The POvIV randomized clinical trial. JAMA Surg. 2025;160(3):276-284. doi:10.1001/jamasurg.2024.6439
- Major Extremity Trauma Research Consortium, O’Toole RV, Stein DM, et al. Aspirin or low-molecular-weight heparin for thromboprophylaxis after a fracture. N Engl J Med. 2023;388(3):203-213. doi:10.1056/NEJMoa2205973