Orthopaedic surgeons often encounter radiographic findings that raise concern for undiagnosed malignancies, with diagnoses ranging from benign bone cysts to metastases or primary bone tumors. Prior classification systems, such as Madewell-Lodwick, indicated that geographic lesions with well-defined borders were generally benign, as opposed to permeative, ill-defined lesions being more concerning. However, there was no comprehensive system for all pertinent imaging findings of potentially malignant lesions. In handling lesions that are most certainly benign or malignant, the decision is simple; but often, orthopaedic surgeons must make an informed decision, based on a combination of history and imaging, whether a patient should undergo further workup or referral to an orthopaedic oncologist. This is one of many reasons why the Bone-RADS score was developed.
What is the Bone-RADS score?
Reporting and data systems (RADs) are consensus guidelines utilized in other organ systems, such as breast cancer, lung cancer, and liver lesions. Teams of experts create these systems to standardize terminology, create reporting templates, and offer management recommendations based on imaging. A Bone-RADS committee was recently organized by the American College of Radiology to create a standardized scoring system for bone lesions.
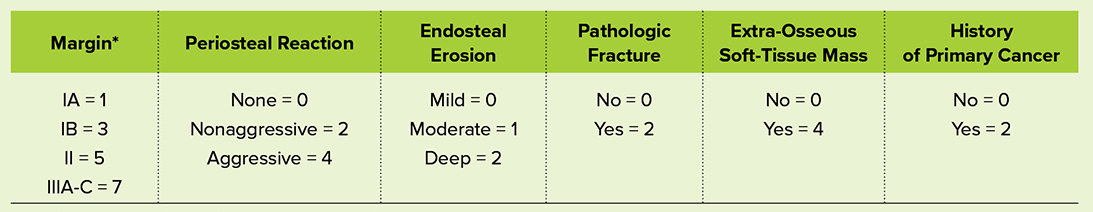
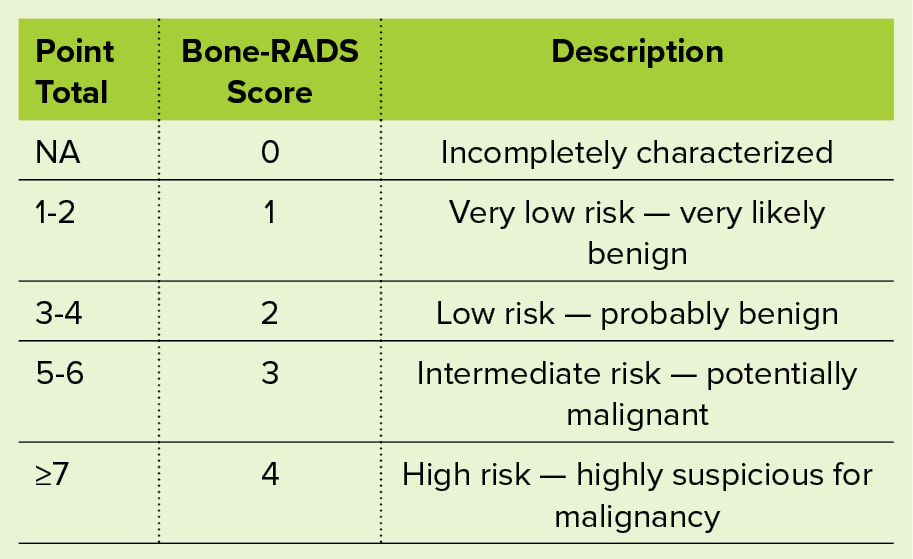
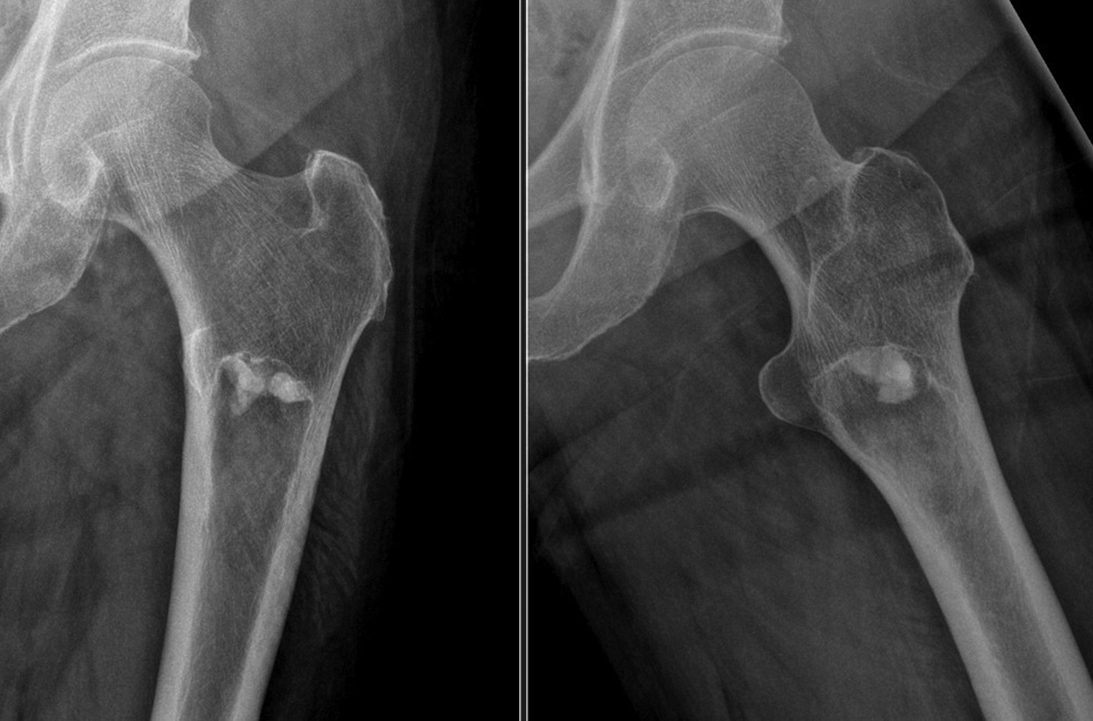
The Bone-RADS score is a numerical scale from 1 to 4 with corresponding risk assignments (very low, low, intermediate, high). The score is based on numerous factors, such as a patient’s imaging and past oncologic history. Radiographic findings that predict risk include margination, pattern of periosteal reaction, depth of endosteal erosion, pathological fracture, and extra-osseus soft-tissue mass (Table 1). Points from each of these categories are summed, and the total corresponds with a Bone-RADS score, with 1-2 meaning very low risk, 3-4 meaning low risk, 5-6 meaning intermediate risk, and 7 meaning high risk of malignancy (Table 2). Management recommendations are made for further surveillance or referral to orthopaedic oncology. The categories of the Bone-RADS score are listed below.
Margin
Lesion margination gives crucial information regarding the biologic activity of a lesion. G.S. Lodwick, MD, was one of the first to show different patterns of bone destruction on radiographs correlated with survival, describing three patterns: geographic, moth eaten, and permeative. He then proposed a grading system which was later expanded by John E. Madewell, MD. Concepts were consolidated in the Modified Lodwick-Madewell classification, still in use today. This classification is used to determine the “margin” category of the Bone-RADS score.
Periosteal reaction
Based on the inciting factor, periosteal reaction corresponds to the underlying lesion’s rate of growth and endosteal forces. Indolent or slow-growing lesions generate solid, smooth periosteal reaction. Lesions that have thin, irregular, or incomplete levels of periosteal reaction are much more concerning because they indicate a more aggressive process that the body cannot respond to quickly. Other descriptors of aggressive types of periosteal reaction include lamellated (like onion skin), spiculated (“hair on end”), and divergent spiculated.
Endosteal erosion
Pressure on the endosteum of bone can arise from bone lesions and is graded in this system by severity (grades 1, 2, and 3). This is based on depth of cortical erosion and is broken into thirds. Grade 1 being one-third, grade 2 being two-thirds, and grade 3 being complete or near-complete erosion.
Pathologic fracture
Associated pathologic fracture is an indicator of the tumor’s destruction of the structural integrity of bone. This is most encountered in metastatic disease. Mirels’ scoring system is commonly used to risk-stratify these metastatic lesions and their risk for pathologic fracture. In the Bone-RADs score, it is a binary “yes” or “no” qualifier.
Management recommendations
The guidelines make recommendations based on the Bone-RADS score to consider surveillance, further imaging, biopsy, or referral to orthopaedic oncology:
- Very low-risk lesions: If asymptomatic, consider workup to be complete versus annual surveillance to ensure expected stability. If symptomatic, or if there is a change in clinical presentation, consider advanced imaging and orthopaedic oncology referral for treatment of benign tumor.
- Low-risk lesions: Proceed with short interval (three- to six-month) surveillance to ensure stability. Consider advanced imaging to assess tumor composition and possibly biopsy to confirm benignity if needed. Consider orthopaedic oncology referral for surveillance or treatment of benign tumor.
- Intermediate-risk lesions: This warrants referral to orthopaedic oncology for probable biopsy and treatment planning. Advanced imaging such as CT, MRI, or bone scan is recommended for further characterization.
- High-risk lesions: Refer to orthopaedic oncology for recommended biopsy and treatment planning. Advanced imaging recommended for tumor staging, including additional potential sites of disease.
Why Bone-RADS matters
One of the main benefits of the Bone-RADS score for orthopaedic surgeons, or any ordering clinician, is that it provides a clear, standardized approach to interpreting imaging findings and recommendations for surveillance or referral. In the radiographic workup of a bone lesion, a radiologist may report the findings using the Bone-RADS scoring system. This shared framework enhances decision-making, allowing for more timely interventions and reducing the likelihood of missing signs of metastatic or primary disease.
For example, a patient with a Bone-RADS score of 3 or 4 might warrant a biopsy or advanced imaging, such as MRI or positron-emission tomography (PET) scans, to confirm the diagnosis of bone metastasis or primary bone malignancy. Alternatively, a score of 1 or 2 may provide the reassurance needed to undergo surveillance unless other symptoms arise. It is important to note that, although the Bone-RADS score aims to risk-stratify radiographic images, its concepts can be applied to advanced imaging studies.
The Bone-RADS score is an exciting and innovative tool that promises to enhance the ability of orthopaedic surgeons to diagnose and properly manage bone lesions based on radiographic features. By providing a standardized and objective approach to interpreting radiologic findings, Bone-RADS provides orthopaedic surgeons and radiologists with an organized system to interpret and communicate imaging findings of bone lesions. Studies are being developed to validate this proposed system with a numerical risk of malignancy, thus providing real-
world validation of this schema. Other future ideas include integration into current or generative artificial intelligence to assist with pattern recognition. As the Bone-RADS score gains wider adoption in clinical practice, it is poised to become a crucial component of cancer care, helping orthopaedic surgeons deliver better, more precise care to patients.
Alec Bigness, MD, is a third-year orthopaedic surgery resident at University of South Florida Department of Orthopaedics.
Jamie Caracciolo, MD, is an associate professor and associate member in the Department of Radiology at Moffitt Cancer Center in Tampa, Florida.
Odion Binitie, MD, FAAOS, is a professor and senior member in the Department of Sarcoma at Moffitt Cancer Center. Dr. Binitie is a member of the AAOS Now Editorial Board.
References
- Lodwick GS, Wilson AJ, Farrell C, Virtama P, Dittrich F. Determining growth rates of focal lesions of bone from radiographs. Radiology. 1980;134(3):577-583. doi:10.1148/radiology.134.3.6928321
- Caracciolo JT, Temple HT, Letson GD, Kransdorf MJ. A modified Lodwick-Madewell grading system for the evaluation of lytic bone lesions. AJR Am J Roentgenol. 2016;207(1):150-156. doi:10.2214/AJR.15.14368