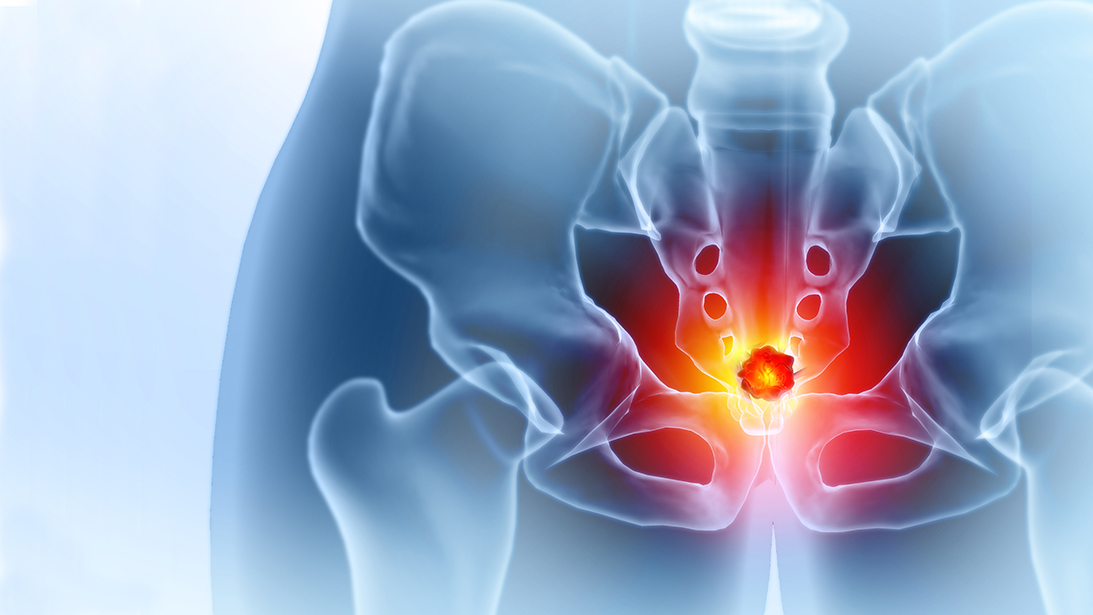
Sacral bone tumors are rare and may be either benign or malignant. Of those that are malignant, metastatic disease (carcinoma or hematologic) far outweighs the number of primary bone malignancies.
Sacral tumors present in four ways: incidentally on imaging; during workup for focal sacrum/posterior pelvic pain; during evaluation for radicular symptoms or sacral nerve dysfunction (including bladder/bowel/sexual function); or for generalized pelvic pain/fullness.
Imaging defines extent and guides biopsy and treatment
While a variety of imaging modalities might initially demonstrate a sacral tumor, CT and MRI are most useful for defining tumor extent and planning treatment. CT provides details about the bony anatomy and can help diagnose a pathologic fracture or aid in surgical planning. MRI is the gold standard for evaluation of bone and soft tissue tumors, as it provides information about the tumor’s makeup, such as water and fat content, areas of viable tumor (e.g., MR enhancing component), and necrotic tissue, typically the MR central non-enhancing component. In the sacrum, MRI also provides a valuable role in assessing the relationship to the neural structures and contrast-enhancement can help identify the vasculature.
Diagnosis requires biopsy. The preferred method is typically via a core needle sample, often performed with CT image guidance. An incisional (open) biopsy is acceptable only if contamination is limited. After diagnosis and staging, treatment depends on tumor type and surgical “resectability.”
Malignant tumors
The most common malignant sacral lesion is metastatic cancer to bone. This typically involves carcinoma metastases—prostate, breast, lung, renal—or hematologic metastases (e.g., myeloma and lymphoma). The treatment of these lesions is almost always palliative, to improve pain and/or function because of tumor invasion, leading to either bone compromise (impending or pathologic fracture) or nerve compression. Metastatic lesions may respond to systemic therapy directed at the metastasizing cancer. Myeloma or lymphoma may respond quickly and dramatically enough to not require any additional treatment.
Palliative radiation therapy is another excellent option to focally treat metastatic disease to improve pain or reduce tumor size and therefore ease nerve compression. On occasion, surgical decompression, with or without instrumentation, may help treat acute nerve compression symptoms. Surgical stabilization may also treat symptoms related to impending or pathological fracture. When possible, percutaneous methods should be employed to reduce the risk for wound complications, particularly in patients on cancer medications that place them at increased risk for wound breakdown (for instance, anti-angiogenic tyrosine kinase inhibitors) or otherwise compromise the immune system (such as antineoplastic chemotherapy).
Chordomas are the most common primary malignancy of the sacrum, accounting for slightly less than half of all primary sacral tumors. Arising from primitive notochordal tissue, chordomas predominantly involve the terminal ends of the spinal column (i.e., sacrococcygeal and skull base regions). Characteristically, chordomas arise from the lower sacrum and present as a midline mass emanating anteriorly into the pre-sacral as illustrated in a pictorial review by Senne and colleagues (See Figure 3: A-F).
Conventional chordomas are typically slow-growing and low grade, but there are more aggressive subtypes (poorly differentiated and de-differentiated), which confer a worse prognosis. Treatment typically involves wide local resection that may require nerve sacrifice and require extensive reconstruction. Recurrence rates can be high due to the difficulty achieving negative margins. Median survival is five to 10 years, with long-term disease-free and overall survival around 50%. Given the morbidity associated with surgical resection of chordomas, radiation may be used as definitive treatment or an adjunct but requires very high doses (>65 Gy) due to the tumor’s radio-insensitivity. At such doses, complications or late effects of radiation are common, can be quite significant, and even may generate a secondary sarcoma. Carbon ion and proton therapy modalities are currently being investigated and may provide a reasonable (or even preferred) alternative for local control.
Primary bone sarcomas of the sacrum
Primary bone sarcomas of the sacrum include chondrosarcoma, osteosarcoma, and Ewing sarcoma. Primary bone sarcomas are more frequently eccentric and more commonly involve the upper segments of the sacrum than distal sacrum/coccyx.
Chondrosarcoma, the most common primary bone sarcoma, is chemo- and radio-insensitive and treated with resection. They tend to affect middle-aged patients with a male predilection.
Osteosarcoma of the axial skeleton is less common than in the appendicular skeleton and often presents in a slightly older age group, also with a slight male predominance. When osteosarcoma does present in the axial skeleton, the lumbosacral spine is the most common location. It is typically high grade and treated with neoadjuvant chemotherapy (cisplatin and doxorubicin +/- methotrexate), followed by surgical resection and then adjuvant chemotherapy. Survival is worse than appendicular disease, with reported long-term survival reported around 30%-40% compared to 60%-70% in the axial skeleton.
Ewing sarcoma is a small round blue-cell tumor. It is, by definition, high grade and represents a clonal expansion resulting from genetic translocation, most commonly between chromosomes 11 and 22 and involving the EWSR1 and FLI1 genes. It is also treated with a standard chemotherapy regimen alternating between VDC (vincristine, doxorubicin, and cyclophosphamide) and IE (ifosfamide and etoposide). Local control can be accomplished with surgical resection or with radiation therapy. In appendicular and pelvic Ewing sarcoma, surgery is considered the gold standard and data suggests improved overall survival, but for Ewing sarcoma of the sacrum, where surgical resection may be far more morbid and survival is worse overall, radiation can be an acceptable alternative and without significant decrease in overall survival.
Surgery may require partial or total sacrectomy, with pelvic or lumbar resection. Morbidity depends on nerve levels, reconstruction feasibility, and perioperative and postoperative complications, which are often quite high.
Benign tumors
While any number of primary benign bone tumors may be possible, the most clinically relevant is giant cell tumor of bone (GCT). These are clinically important because they are locally aggressive lesions that often require intervention, given their predilection to grow large and destroy bone. GCTs typically afflict young adults and are more common in women. GCT of the spine is rare, but when it occurs, it is most frequently in the sacrum. As GCTs do in other locations, they often present eccentrically and can have a leading edge of aggressive osteolysis.
Since they are benign lesions, wide resection is not necessary, and the preferred treatment, when feasible, is extended curettage with local adjuvant therapy and bone grafting or cementation, with or without internal fixation. Recurrence rates can be high, and GCTs require postoperative surveillance, like a malignant lesion. Denosumab is an option when surgery is too morbid.
Sacral tumors demand precise imaging, biopsy, and multidisciplinary planning to balance oncologic control with nerve preservation and patient function. Advances in surgical techniques, systemic therapy, and radiation have improved options, but treatment decisions must be individualized based on tumor biology, anatomy, and patient goals.
Russell Stitzlein, MD, is a fellowship-trained orthopaedic oncologist who is an Associate Clinical Professor and serves as the Associate Residency Program Director and Chief of Orthopaedic Oncology & Sarcoma Surgery at the University of California, Irvine – UCI Health Medical Center.
References
- Varga PP, Bors I, Lazary A. Sacral tumors and management. Orthop Clin North Am. 2009;40(1):105-123, vii. doi:10.1016/j.ocl.2008.09.010.
- Senne J, Nguyen V, Staner D, Stensby JD, Bhat AP. Demystifying sacral masses: a pictorial review. Indian J Radiol Imaging. 2021;31(1):185-192. doi:10.1055/s-0041-1729766.
- Yu X, Kou C, Bai W, et al. Comparison of wide margin and inadequate margin for recurrence in sacral chordoma: a meta-analysis. Spine (Phila Pa 1976). 2020;45(12):814-819. doi:10.1097/BRS.0000000000003386.
- Santoro A, Totti R, El Motassime A, et al. Carbon ion and proton therapy in sacral chordoma: a systematic review. J Clin Med. 2025;14(17):5947. doi:10.3390/jcm14175947.
- Bielack SS, Kempf-Bielack B, Delling G, et al. Prognostic factors in high-grade osteosarcoma of the extremities or trunk: an analysis of 1,702 patients treated on neoadjuvant cooperative osteosarcoma study group protocols. J Clin Oncol. 2002;20(3):776-90. doi:10.1200/JCO.2002.20.3.776.