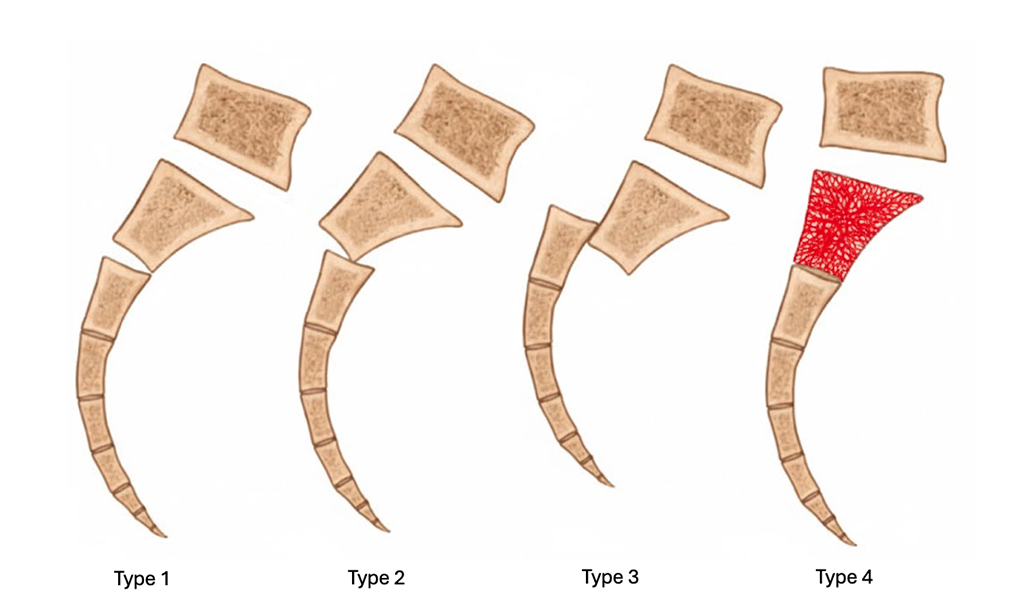
Type 1 – non-displaced; Type 2 – angulated; Type 3 – completely displaced; Type 4 – impacted.
Although sacral fractures are uncommon, their transverse variants pose unique challenges. These injuries, often linked to high-energy trauma or severe falls, can lead to complex spinopelvic dissociation and carry a significant risk of neurologic complications—making early recognition and management critical.
Sacral fractures are often identified in the setting of pelvic ring injuries such as lateral compression injuries. An even rarer subset of sacral fractures, those with a transverse fracture pattern, can be seen in isolation or more commonly with bilateral longitudinal fractures resulting in a form of spinopelvic dissociation (SPD). Unlike lateral compression injuries, transverse sacral fractures can result from a high energy axial load injury (e.g., fall from height, suicide jumper) or a ground-level fall directly onto the buttock with the former seen more often in younger patients and the latter in older patients with osteoporotic bone.
Transverse sacral fractures are considered Denis zone III injuries given that the fracture traverses across the sacral body. The horizontal nature of these fractures can result in unique deformities of the sacrum — anterior-posterior translation of the distal segment and/or increased kyphosis of the sacrum as classified by Roy-Camille et al. (Figure 1). Due to the proximity of the cauda equina and the central sacral canal, significantly displaced or angulated transverse sacral fractures can result in varying degrees of neurologic issues ranging from sensorimotor deficits in the lower extremities, erectile dysfunction in males or dyspareunia in females, fecal or urinary incontinence, or emergent cauda equina syndrome. The rate of neurological deficit varies widely across the literature, but the two largest studies in the past 10 years reported post-traumatic deficits in 33%-62% of patients.
Before discussing the neurologic sequelae of transverse sacral fractures, it is important to understand that sacral nerve roots (S2-S4) have a significant role in bowel and bladder function. Specifically, these nerve roots relay sensory information (e.g., full bladder or rectum), control the muscles of the pelvic floor in addition to both urethral and anal sphincters, and contract the detrusor muscle of the bladder and muscles of the rectum. With regards to sexual function, the pelvic splanchnic nerves relay the parasympathetic signals responsible for initiating an erection while the pudendal nerve conveys sensation from the penis and motor function of the pelvic floor muscles that maintain an erection and promote ejaculation. In females, these nerves carry sensory signals from the genitals for sexual arousal and play a role in pelvic floor muscle and uterine function during childbirth.
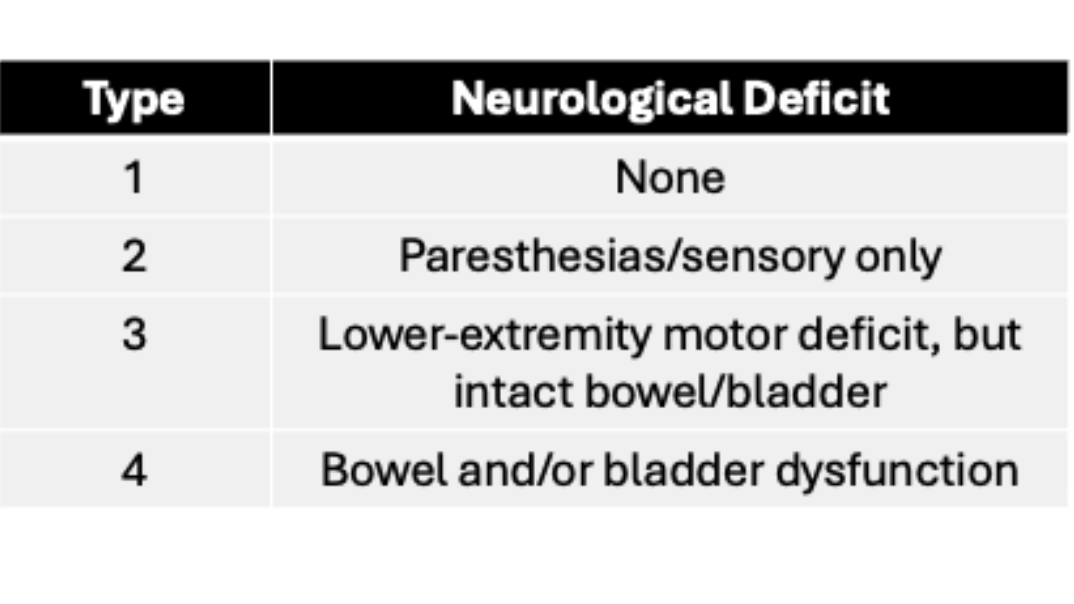
In the setting of a fracture, the severity of neurological deficit may be difficult to ascertain, particularly with concomitant pain or if the patient is intubated and sedated. But evaluation of neurological function in both the acute and sub-acute setting includes usage of the Gibbons classification (Table 1) and structured patient interviews regarding urinary, bowel, and sexual function. One consideration to keep in mind is that higher energy injuries such as jumping from height seem to predominantly affect the upper sacral levels (S1-S2), whereas lower-energy injuries affect the lower sacral levels (S3–S5). Regardless of the mechanism of injury, however, the severity of the sacral kyphosis and overt injury to the nerve roots may be the most important determinants of neurologic dysfunction regardless of bony healing.
Treatment options
Treatment for these injuries range from nonoperative to operative management with most studies advocating for surgical intervention, especially for unstable fracture patterns (e.g., SPD). Lumbopelvic fixation with or without iliosacral screws is the suggested construct for SPD while isolated transverse sacral fractures may be amenable to iliosacral screws alone if the fracture is in the upper sacral segments. Decompression of nerve roots with laminectomy has also been described, but studies suggest that deformity reduction and fracture stabilization are more likely to result in neurologic recovery compared to isolated decompression.
With appropriate treatment, outcomes are favorable for improvement of neurologic function. In the largest systematic review of transverse sacral fractures in 2018, Kempen et al. reported recovery of at least one Gibbons type (Table 1) in 58% of the nonoperatively treated patients and 63% in those treated surgically. Even in patients with identified root injuries or lacerations, 46% regained bladder and bowel control. These findings are similar to a more recent review by Morris et al. in 2023 where they looked at SPDs treated with surgery and observed complete neurologic recovery in 58% of cases at an average of 203 days of follow-up. Slightly less than 10% of their patients had persistent bowel or bladder dysfunction (4 out of 45), and they reported radiculopathy as the most common persistent neurologic issue. Sacral neuromodulation, a percutaneous nerve stimulator procedure performed by urologists, may be an effective adjunctive treatment as it has been described for the treatment of chronic pelvic pain, chronic fecal incontinence, overactive bladder, and possibly sexual dysfunction. However, this treatment requires the presence of at least one intact S3 nerve root and, thus, would not be efficacious in patients with known bilateral S3 nerve root disruptions.
In summary, although transverse sacral fractures and SPDs are rare injuries, they can result in a high rate of genitourinary or bowel dysfunction, particularly those fractures with severe kyphosis, complete displacement of bony fragments into the sacral canal, or traumatically disrupted nerve roots. Nonoperative treatment is an option for stable fracture patterns and shown to have favorable results with eventual return of neurologic function in >50% of patients. Reduction and subsequent stabilization with or without decompression of these fractures portend the best outcomes at an average of six months after surgery. The identification of these Denis zone III fractures is paramount based on imaging, which may demonstrate a paradoxical inlet on an AP pelvis or acute angle kyphosis on sagittal CT images. Although the exact timing to surgery has not been established, early surgical intervention should be considered for unstable patterns (e.g., SPD) or those with acute neurologic compromise with hyperkyphosis on imaging.
Philip K. Lim, MD, is an associate professor in the department of Orthopaedics UCI Health, Orange, California. He received trauma fellowship training at UT Houston and did his residency at UCI Health.
References
- Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988;(227):67-81. doi:10.1097/00003086-198802000-00010. 1.
- Roy-Camille R, Saillant G, Gagna G, Mazel C. Transverse fracture of the upper sacrum. Suicidal jumper’s fracture. Spine (Phila Pa 1976). 1985;10(9):838-845. doi:10.1097/00007632-198511000-00011.
- Kempen DHR, Delawi D, Altena MC, Kruyt MC, van den Bekerom MPJ, Oner FC, Poolman RW. Neurological outcome after traumatic transverse sacral fractures: a systematic review of 521 patients reported in the literature. JBJS Rev. 2018;6(6):e1. doi:10.2106/JBJS.RVW.17.00115.
- Morris CA, Moo Young JP, Savakus JC, Obey MR, Pereira DE, Hills JM, McKane A, Babcock SN, Miller AN, Stephens BF, Mitchell PM. Neurologic injury after spinopelvic dissociation: incidence, outcome, and predictors. Injury. 2023;54(2):615-619. doi:10.1016/j.injury.2022.10.008.
- Urzúa A, Marré B, Martínez C, Ballesteros V, Ilabaca F, Fleiderman J, Zamorano JJ, Yurac R, Lecaros M, Munjin M, Lahsen P. Isolated transverse sacral fractures. Spine J. 2011;11(12):1117-1120. doi:10.1016/j.spinee.2011.11.004.
- Schildhauer TA, Bellabarba C, Nork SE, Barei DP, Routt ML Jr, Chapman JR. Decompression and lumbopelvic fixation for sacral fracture-dislocations with spino-pelvic dissociation. J Orthop Trauma. 2006;20(7):447-457. doi:10.1097/00005131-200608000-00001.
- de Oliveira PS, Reis JP, de Oliveira TR, Martinho D, E Silva RP, Marcelino J, Gaspar S, Martins F, Lopes T. The impact of sacral neuromodulation on sexual dysfunction. Curr Urol. 2019;12(4):188-194. doi:10.1159/000499307.