Patient-reported outcome measures (PROMs) have become an essential component of modern healthcare delivery and evaluation. Unlike traditional clinical outcomes, which rely on data collected from physicians such as imaging, laboratory values, or the presence of complications, PROMs capture the patient’s perspective on their health, functional status, and quality of life. These measures reflect how patients experience disease and the ensuing treatment, offering a more complete understanding of care outcomes. In clinical practice, PROMs are increasingly used to inform decision making at the point of care. They can guide conversations between clinicians and patients, help inform risk and benefit conversations, and identify concerning clinical issues that may not otherwise surface.
Given these clinical benefits and the evolution toward patient-centered and accountable care, policy changes are accelerating the integration of PROMs into routine practice. The Centers for Medicare & Medicaid Services (CMS) have introduced Patient-Reported Outcome-Based Performance Measures (PRO-PMs) and the Transforming Episode Accountability Model (TEAM). These initiatives require healthcare organizations to collect and report standardized PROM data as part of reimbursement and performance evaluation frameworks for orthopaedic conditions including total hip and total knee arthroplasty.
However, the measurement and integration of PROMs into care can be challenging. For example, literature demonstrates that at one-year postoperatively, collection rates at many centers are only 20-40%. The 2024 American Joint Replacement Registry Annual Report reveals a 25-32% one-year PROM response rate from patients undergoing primary hip or knee arthroplasty. PROMs aim to place patients at the center of care, but current systems do not provide the information nor the tools to make this simple. Integrating PROMs into clinical care without proper education and closed care feedback would be akin to ordering radiographs or a lab value and not explaining to a patient why it is being ordered nor discussing the results. Further, evidence demonstrates that patients not only want to be involved in the decision-making process, but such involvement improves their confidence in the decision and perceived quality of care. As AAOS aims to ensure patients remain at the center of their care discussions, the organization should empower patients with the information and tools they need to make the best decisions.
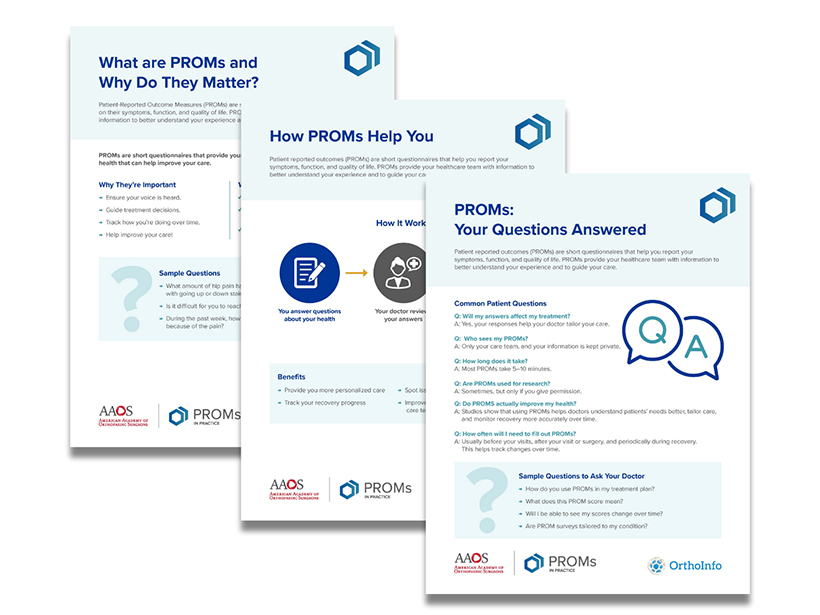
The AAOS Committee on Healthcare Safety, which will soon formally integrate the PROMs Workgroup, has developed patient-facing educational resources to increase PROMs awareness and understanding. These resources are designed to support meaningful conversations between patients and their care teams about how PROMs contribute to high-quality, patient-centered orthopaedic care. These materials include a fact sheet that explains what PROMs are, why they matter, and what patients should know before completing them; a set of frequently asked questions and a conversation guide outlining key questions patients may ask their clinician about completing PROMs and interpreting their results; and an infographic that visually walks patients through the process and benefits of participating in PROM data measurement. The information is hosted on OrthoInfo’s new PROMs-dedicated page.
These resources directly support the AAOS Strategic Plan’s Patient Goal, which emphasizes empowering patients to take an active role in their musculoskeletal health. By helping patients understand their experiences and outcomes, these materials foster greater transparency, trust, and collaboration between patients and their orthopaedic teams. Ultimately, the Committee on Healthcare Safety hopes these resources will encourage patients to engage more fully in their care, align treatment decisions with their personal values and goals, and contribute to improved overall outcomes and satisfaction.
Readers are encouraged to visit the OrthoInfo and AAOS PROMs web pages to learn more and access these patient educational materials.
Lauren Shapiro, MD, MS, is a hand and upper extremity surgeon and health services researcher at the University of California, San Francisco. She currently serves on the Committee on Evidence-Based Quality and Value and the AAOS PROMs Workgroup, and she is the incoming PROMs Section Leader for the AAOS Committee on Healthcare Safety.
Jennifer Rivera, MBA, is a staff member at AAOS and the liaison to the Committee on Healthcare Safety.
References
- Greenhalgh J, Long AF, Flynn R. The use of patient reported outcome measures in routine clinical practice: Lack of impact or lack of theory? Soc Sci Med. 2005;60:833-843. doi:10.1016/j.socscimed.2004.06.022
- Basch E, Deal AM, Kris MG, et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: A randomized controlled trial. J Clin Oncol. 2016;34:557-565. doi:10.1200/JCO.2015.63.0830
- Jayakumar P, Moore MG, Furlough KA, et al. Comparison of an artificial intelligence-enabled patient decision aid vs educational material on decision quality, shared decision-making, patient experience, and functional outcomes in adults with knee osteoarthritis: A randomized clinical trial. JAMA Netw Open. 2021;4:e2037107. doi:10.1001/jamanetworkopen.2020.37107
- Bernstein DN, Fear K, Mesfin A, et al. Patient-reported outcomes use during orthopaedic surgery clinic visits improves the patient experience. Musculoskeletal Care. 2019;17:120-125. doi:10.1002/msc.1379
- TEAM (Transforming Episode Accountability Model). CMS.gov. July 31, 2025. Accessed Oct. 31, 2025. www.cms.gov/priorities/innovation/innovation-models/team-model
- Reporting of the THA/TKA PRO-PM. CMS.gov. Accessed Oct. 20, 2025. https://qualitynet.cms.gov/inpatient/measures/THA_TKA.
- Rullán PJ, Pasqualini I, Zhang C, Klika AK, Piuzzi NS; The Cleveland Clinic OME Arthroplasty Group. How to raise the bar in the capture of patient-reported outcome measures in total joint arthroplasty: results from active and passive follow-up measures. J Bone Joint Surg Am. 2024;106(10):879-890. doi:10.2106/JBJS.23.00558
- Burnett RA, Blackburn BE, Archibeck MJ, et al. Insufficient mandatory patient-reported outcome rates at an academic hospital despite increased resource allocation. J Arthroplasty. 2025;40(9S1):S137-S141. doi:10.1016/j.arth.2025.05.030
- American Joint Replacement Registry 2024 Annual Report. AAOS. Accessed Oct. 31, 2025. www.aaos.org/registries/publications/ajrr-annual-report/
- Driever EM, Stiggelbout AM, Brand PLP. Patients’ preferred and perceived decision-making roles, and observed patient involvement in videotaped encounters with medical specialists. Patient Educ Couns. 2022;105(8):2702-2707. doi:10.1016/j.pec.2022.03.025
- Dardas AZ, Stockburger C, Boone S, An T, Calfee RP. Preferences for shared decision making in older adult patients with orthopedic hand conditions. J Hand Surg Am. 2016;41(10):978-987. doi:10.1016/j.jhsa.2016.07.096
- Burton D, Blundell N, Jones M, Fraser A, Elwyn G. Shared decision-making in cardiology: do patients want it and do doctors provide it? Patient Educ Couns. 2010;80(2):173-179. doi:10.1016/j.pec.2009.10.013
- Heisler M, Vijan S, Anderson RM, Ubel PA, Bernstein SJ, Hofer TP. When do patients and their physicians agree on diabetes treatment goals and strategies, and what difference does it make? J Gen Intern Med. 2003;18(11):893-902. doi:10.1046/j.1525-1497.2003.21132.x
- Kremer H, Ironson G, Schneiderman N, Hautzinger M. “It’s my body”: does patient involvement in decision making reduce decisional conflict? Med Decis Making. 2007;27(5):522-532. doi:10.1177/0272989X07306782
- Lantz PM, Janz NK, Fagerlin A, Schwartz K, Liu L, Lakhani I, et al. Satisfaction with surgery outcomes and the decision process in a population-based sample of women with breast cancer. Health Services Research. 2005;1;40(3):745-768.
- Solberg LI, Crain AL, Rubenstein L, Unützer J, Whitebird RR, Beck A. How much shared decision making occurs in usual primary care of depression? J Am Board Fam Med. 2014;27(2):199-208. doi:10.3122/jabfm.2014.02.130164
- Tambuyzer E, Van Audenhove C. Is perceived patient involvement in mental health care associated with satisfaction and empowerment? Health Expect. 2015;18(4):516-526. doi:10.1111/hex.12052