There have been significant advancements in orthopaedic oncology in recent years, such as the identification of new tumor types, reclassification or removal of existing types, and numerous discoveries that simplify diagnosis and increase treatment options. Keeping up with this rapidly evolving field can be challenging for surgeons at all levels of practice, making concise summaries and reviews invaluable.
New tumor types
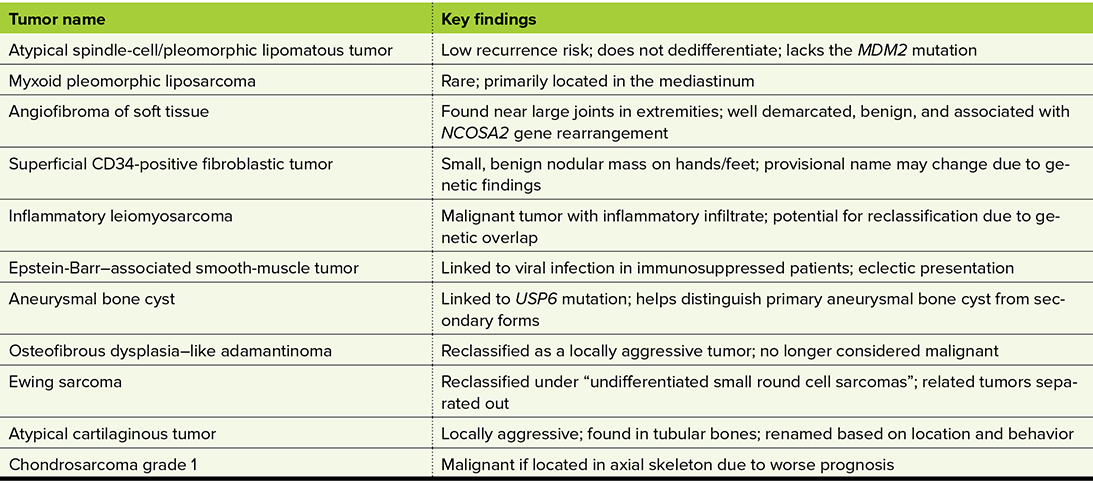
The latest edition of the “World Health Organization Classification of Tumors: Soft Tissue and Bone Tumors,” published in 2020, introduced several newly recognized soft-tissue and bone tumors (Table 1). Among them is the atypical spindle-cell/pleomorphic lipomatous tumor, a lesion composed of diverse cell types (hence the name “pleomorphic”), which has a low recurrence risk. Unlike the more common atypical lipomatous tumor, this entity does not dedifferentiate into malignancy or harbor the MDM2 mutation.
Another addition is myxoid pleomorphic liposarcoma; however, this tumor should be of little concern for orthopaedic surgeons as it is mostly found in the mediastinum. Angiofibroma of soft tissue is also newly classified; it typically arises near large joints in the extremities, is benign and well demarcated, and often harbors an NCOR2 gene rearrangement.
Superficial CD34-positive fibroblastic is a provisional name assigned to a tumor that presents as a benign nodular mass in the hands or feet. This is one to keep under the radar because its name may soon change given its frequent association with another genetic rearrangement.
And lastly, within the category of smooth-muscle tumors, two new entities have been described. Inflammatory leiomyosarcoma is a malignant tumor commonly found in the deep lower extremities of young to middle-aged individuals. Microscopically, it shows inflammatory infiltrate and shares genetic features with another rare tumor, rhabdomyoblastic tumor, suggesting it may eventually be reclassified. The second addition in this category is Epstein-Barr virus–associated smooth-muscle tumor, linked to Epstein-Barr virus infection in immunosuppressed patients. This tumor can present in various clinical scenarios, including primary immunodeficiency, HIV infection, and post-transplantation, with an eclectic array of manifestations.
Bone and cartilage tumors
In bone tumors, several entities have been renamed, reclassified, or removed. Aneurysmal bone cysts, giant-cell tumors of bone, and non-ossifying fibromas now fall under the category of osteoclastic giant cell–rich tumors of benign nature. It is worth noting that a genetic marker, ubiquitin-specific peptidase 6 (USP6), has been previously linked to primary aneurysmal bone cysts, facilitating their diagnosis and aiding in distinguishing them from secondary lesions associated with tumors such as chondroblastoma and giant-cell tumor of bone.
Simple bone cysts, fibrous dysplasia, and osteofibrous dysplasia now fall under the category of other mesenchymal tumors of bone, with osteofibrous dysplasia–like adamantinoma reclassified as locally aggressive rather than malignant. Meanwhile, classic and de-differentiated adamantinomas remain malignant. Ewing sarcoma, previously classified as a miscellaneous tumor, has been reassigned to undifferentiated small round-cell sarcomas. This new grouping includes tumors previously thought to be related to Ewing sarcoma, such as CIC-rearranged sarcoma and sarcoma with BCOR alterations, now recognized as distinct entities.
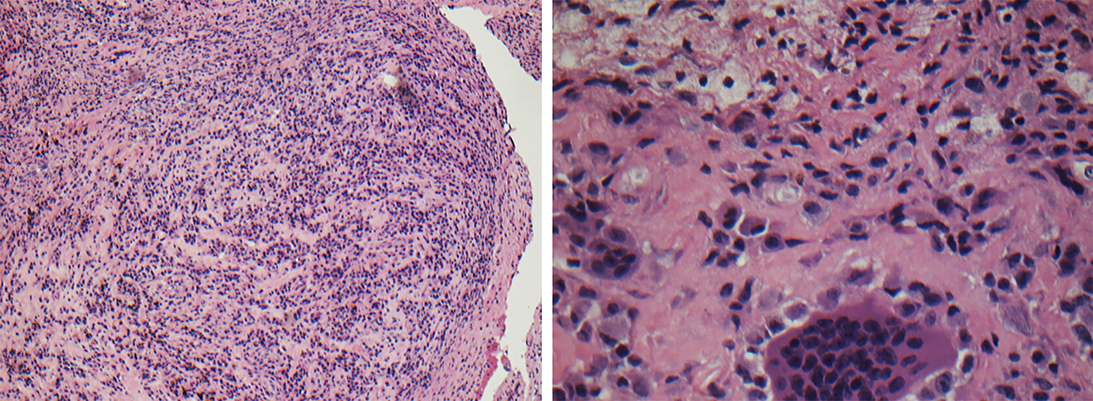
Cartilage tumors have also undergone renaming. Tumors that lie between benign enchondromas and malignant chondrosarcomas are now classified based on their location. When found in tubular bones, they are termed atypical cartilaginous tumors and considered locally aggressive (Figure 1). If similar tumors occur in axial skeleton sites, such as the pelvis or scapula, they are classified as chondrosarcoma grade 1 and considered malignant due to their worse prognosis.
Several tumors have been removed from classifications entirely, including calcifying fibrous tumor, clear-cell osteosarcoma, benign fibrous histiocytoma, and liposarcoma of bone. These overall changes often stem from advances in diagnostic methods that allow previously unrecognized tumor features to prompt the emergence of new tumors, reclassification, or removal.
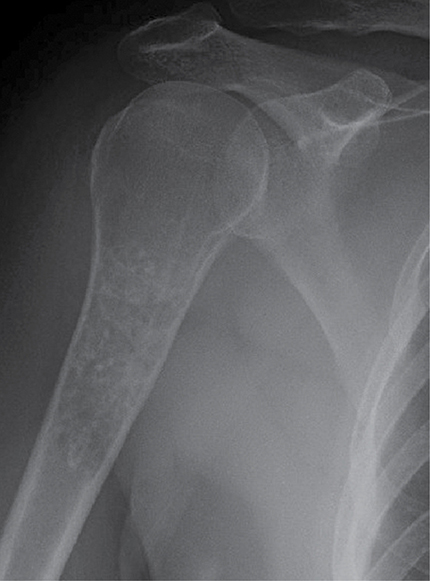
A not-so-recent example is malignant fibrous histiocytoma, which was removed from classifications after research demonstrated that it did not originate from histiocytes. Similarly, pigmented villonodular synovitis is now more accurately named tenosynovial giant-cell tumor, reflecting its origin (Figure 2).
Advances in genetic research
Genetic research continues to transform the field of orthopaedic oncology by improving diagnostic precision and expanding therapeutic options. Mutations such as IDH1/2 assist in identifying chondrosarcomas, whereas H3F3A and H3F3B mutations are associated with giant-cell tumors of bone and chondroblastomas, respectively. The GRM1 mutation has been identified in chondromyxoid fibromas, further aiding in their diagnosis. In soft-tissue tumors, specific gene fusions have also been identified, such as COL1A1-PDGFB in dermatofibrosarcoma protuberans, EWSR1-ATF1 in clear-cell sarcoma, and PAX3/7-FOXO1 in alveolar rhabdomyosarcoma.
Some mutations have even been recognized as potential treatment targets. For instance, the ASPSCR1-TFE3 fusion in alveolar soft-part sarcoma shows sensitivity to anti-angiogenic therapies, whereas the ETV6-NTRK3 fusion in infantile fibrosarcoma makes these tumors responsive to tropomyosin receptor kinase inhibitors.
In summary, advancements in the field of orthopaedic oncology bring hope to patients with rare and challenging conditions. Although the study of bone and soft-tissue tumors is often hindered by limited patient numbers, logistical challenges, and funding constraints, dedicated researchers continue to drive innovation. These discoveries not only deepen the understanding of these complex tumors but also pave the way for breakthroughs in diagnostics, treatment, and overall patient outcomes.
The future of orthopaedic oncology is brimming with potential. With ongoing innovation and collaboration, orthopaedic oncology is transforming patient care, turning once-impossible outcomes into achievable realities, and delivering hope for a better future.
Cecilia Belzarena, MD, MPH, MBA, is an orthopaedic oncologist, pediatric orthopaedic surgeon, and chief of musculoskeletal oncology at the University of Missouri.
Reference
- World Health Organization: WHO Classification of Tumors: Soft Tissue and Bone Tumors. 5th ed. International Agency for Research on Cancer; 2020.