An ePoster presented at the AAOS 2025 Annual Meeting reported practice trends for management of pediatric diaphyseal femoral shaft fractures among pediatric surgeons practicing in North America.
According to study coauthor Alyssa Barre, MD, orthopaedic surgery resident at the University of Kentucky College of Medicine, “The current AAOS Clinical Practice Guidelines (CPGs) lack [a significant number of high-]quality studies to provide strong recommendations for the treatment of pediatric femur fractures. Based on discussions at national meetings and Pediatric Orthopaedic Society of North America (POSNA) work groups, there was a feeling that practice patterns may vary.”
For this study, the POSNA Quality, Safety, and Value Initiative Committee conducted a 12-question survey of all active POSNA members in North America regarding treatment of pediatric femoral shaft fractures. In total, 226 responses were collected. Answers were compared in relation to recommendations in CPGs. Trends in treatment were identified based on surgeon characteristics, including geographical region and age. Surgeon ages were grouped accordingly: 30 to 39 years, 40 to 49 years, 50 to 59 years, and 60 years or older.
“Our study found that treatment preferences of pediatric diaphyseal femur fractures vary uniquely based on surgeons’ age, their geographic region of practice, and the type of practice setting,” Dr. Barre reported. “In general, older surgeons choose from a broader array of treatment options, whereas younger surgeons more frequently choose the current ‘textbook’ options. Academic surgeons were less likely to choose nonoperative choices for some age groups than community/private practice or military surgeons. Region of practice in the Northern Hemisphere influenced patterns as well.”
Age-based variation
Treatment also depended on patient age. For patients aged 0 to 6 months, the most common treatment was a Pavlik harness, with 204 respondents reporting that option. Pavlik harness use decreased and spica cast use increased with increasing surgeon age. Surgeons in the West were less likely to use a Pavlik harness.
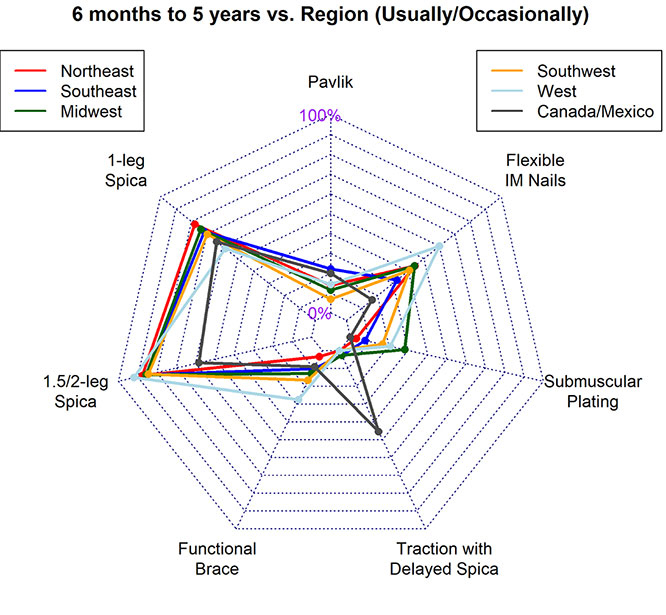
For patients aged 6 months to 5 years, spica casting was the most common treatment, with 175 respondents reporting that option. Surgeons aged 60 years or older were more likely to use flexible intramedullary nails (FINs) in this age range, and surgeons from Canada or Mexico were more likely to choose traction with delayed spica. Submuscular plating was more commonly reported by surgeons in the Midwest, West, and Southwest. Figure 1 shows geographical variations in treatment type used in this patient age range.
For patients aged 5 to 11 years with length-stable fractures, FIN was the most common treatment, with 219 respondents reporting use of that option. Older surgeons and surgeons from academic centers were more likely to choose a nonoperative option. For patients in this age range with length-unstable fractures, submuscular plating was the most common treatment (169 respondents), followed closely by FIN (152 respondents) and rigid intramedullary nailing (122 respondents). For this indication, academic centers were less likely to choose nonoperative options than private practice or military settings. Finally, among children aged 11 to 18 years, rigid intramedullary nailing was the most common treatment, with 221 (98%) of respondents reporting that choice.
Clinical takeaways and next steps
Dr. Barre told AAOS Now Daily Edition, “Our study found a few areas where there was a good bit of variability in practice patterns among surgeons or where preferences stray from our clinical practice guidelines. Surgeons’ ages, their practice location, and their practice type may play into their preferences, and further studies are needed in the identified areas of variability.”
Additionally, Dr. Barre added, “There were a few outliers in our data that we found surprising, such as a handful of people who answered that they usually treat length-unstable femur fractures in patients aged 5 to 11 years with a spica cast.”
She acknowledged that the study is limited by its use of survey data, as well as the fact that the respondents may not represent all practicing pediatric orthopaedic surgeons. Additionally, “Our study shows that surgeons are addressing pediatric femur fractures in a variety of ways, but it lacks any outcomes data,” Dr. Barre noted. “Comparative studies that could determine if one treatment option is superior to another would be beneficial to help strengthen the AAOS CPGs.”
Dr. Barre’s coauthors of “Practice pattern trends among pediatric orthopaedic surgeons for the treatment of femoral shaft fractures” are Andrew Kirk, MD; Gregory S. Hawk, PhD; Jonathan David Grabau, MD; Matthew Halsey, MD, FAAOS; and Vincent W. Prusick, MD, FAAOS.
Rebecca Araujo is the managing editor of AAOS Now. She can be reached at raraujo@aaos.org.