Editor’s note: The following article is a review of a video available via the AAOS Orthopaedic Video Theater (OVT). AAOS Now routinely reviews OVT Plus videos, which are vetted by topic experts and offer CME. For more information, visit aaos.org/OVT.
Anterior cruciate ligament (ACL) injuries are among the most common knee injuries in the active population. The standard treatment for most ACL tears is ligament reconstruction with tendon graft. However, with advancements in surgical techniques, arthroscopic instrumentation, and biologics to enhance healing, primary repair of the injured ACL is emerging as a viable treatment. Most studies have identified proximal ACL tears (Sherman type I or II) as likely the ideal candidates for possible primary repair. Gee et al. found that the incidence of proximal avulsion type tears is estimated to occur in 16%-30% of ACL tears.
In the OVT video titled “ACL repair with BioBrace augmentation and BEAR implant,” Charles Chun-Ting Lin, MD, and colleagues highlight one ACL primary repair strategy for a proximal ACL avulsion. The video begins by providing the background literature on primary ACL repair and its potential advantages relative to ACL reconstruction. Included in this literature review are discussions about the different classification types of ACL tears and the material composition of the BioBrace, a collagen matrix that is embedded with bioabsorbable poly(L-Lactide) (PLLA) microfilaments, and the Bridge-Enhanced ACL Restoration (BEAR) implant, which is a decellularized, bovine-derived, type I collagen.
Proper patient selection and counseling are imperative. The authors highlight the use of this operative technique in a patient, aged 46 years, who sustained a skiing injury to the right knee. In addition to the proximal ACL tear, the patient sustained injuries of the medial collateral ligament and lateral meniscus. The authors discuss operative treatment options in this patient scenario, including ACL reconstruction versus primary ACL repair and partial meniscectomy versus meniscus repair.
The surgical technique begins with diagnostic arthroscopy to confirm that the ACL tear type is compatible with a primary repair. The video demonstrates a proximal avulsion of the native ACL that is reducible to its native footprint on the lateral wall of the intercondylar notch. A radial tear of the lateral meniscus is also identified, and this is repaired with an all-inside meniscal repair strategy.
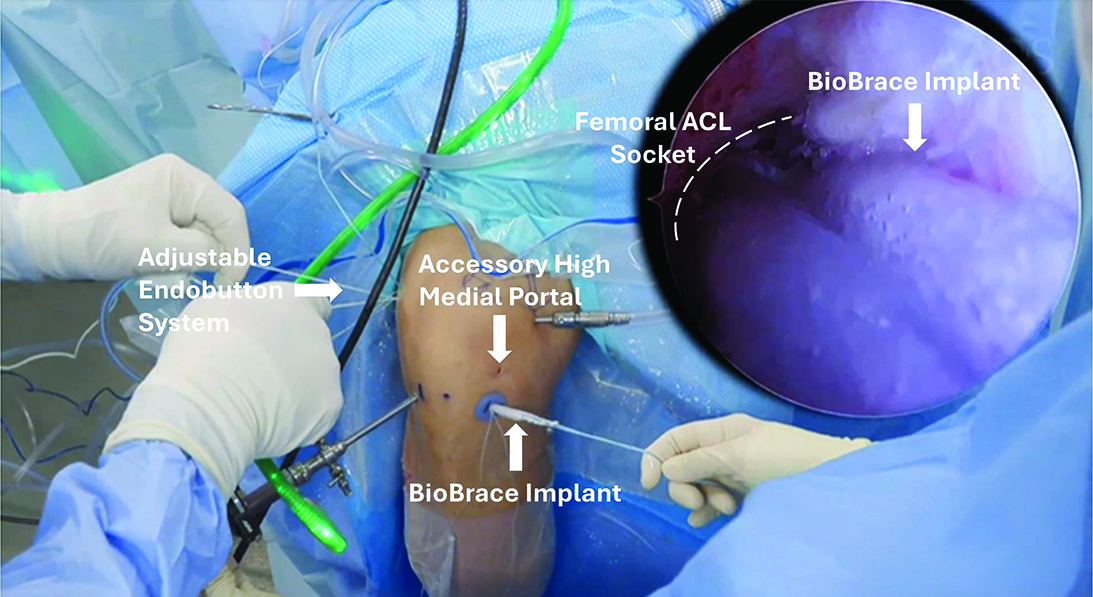
Attention turns back to the surgical repair. The femoral bony footprint is prepared for the primary repair. A soft cannula is placed in the anteromedial arthroscopic portal, and an accessory high medial portal is established for suture management. The native ACL is then whipstitched with a self-retrieving suture passer to get traction control of the native ACL stump. The limbs of the suture used to whipstitch the native ligament are docked in the high medial accessory portal. The authors utilize an outside-in technique to create a 6 mm socket within the native ACL femoral footprint. A passing suture is placed through the 6 mm femoral socket and retrieved out of the soft cannula along the anteromedial portal.
The BioBrace implant is prepared externally with whipstitches on both ends for im plantation. An adjustable loop Endobutton system is passed through the previously established femoral socket, flipped, and docked along the lateral surface of the distal femoral cortex. One limb of the whipstitch in the native ACL along with the BioBrace is then incorporated into the adjustable loop. As the loop comes into the joint, the whipstitch limbs within the native ACL are tied to secure them to the Endobutton system. The native ACL and the BioBrace are tensioned to the native femoral footprint of the ligament by tensioning the loop system (Figure 1).
Excess suture limbs from the native ACL are trimmed flush to the lateral wall of the intercondylar notch. A small separate anterior medial tibial incision is made, which allows a tibial guide to establish a 6 mm transosseous tunnel into the native tibial ACL footprint. The BioBrace implant is then passed into the tibial tunnel, and the tibial fixation of the implant is achieved with a 7 mm PEEK (polyetheretherketone) interference screw.
At this point, the BEAR implant is hydrated with autologous blood from the patient and delivered via a customized syringe system into the intercondylar notch. The video outlines the postoperative rehabilitation protocol, which has initial weight-bearing restrictions for the first four weeks, use of a hinged knee brace, and prescribed progression of knee range of motion. Gradual progression and return to athletic activity are permitted in about four to six months, depending on the rehabilitation progress of the patient.
The conclusion of the video summarizes the initial published clinical cohort outcome data with the BEAR system. Included in the final discussion are the authors’ insights and cautions, including the importance of careful patient selection for this technique and an adequate native ACL stump for the primary repair.
Overall, this video highlights the relevant patient considerations for primary ACL repair versus reconstruction. It provides one of many different strategies to achieve a primary repair using modern instrumentation and biologics. It therefore has educational value for surgeons who may be evaluating the evidence and techniques for ACL repair.
Richard Ma, MD, is the Gregory L. and Ann L. Hummel Distinguished Professor and director of sports medicine in the Department of Orthopaedic Surgery at the University of Missouri. He also serves as a member of the AAOS Now Editorial Board.
Reference
- Gee MSM, Peterson CDR, Zhou ML, Bottoni CR. Anterior cruciate ligament repair: historical perspective, indications, techniques, and outcomes. J Am Acad Orthop Surg. 2020;28(23):963-971. doi:10.5435/JAAOS-D-20-00077
Video details
Title: ACL repair with BioBrace augmentation and BEAR implant
Authors: Charles Chun-Ting Lin, MD; Robert J. Meislin, MD, FAAOS; Jose R. Perez, MD
Published: March 1, 2025
Time: 8:04
Tags: Sports medicine, Knee ligament injuries
Visit aaos.org/OVT to view this award-winning title and more than 1,600 other videos from across orthopaedic topics, institutions, practice management, and industry.