Trouble sleeping is common in the period immediately after total hip arthroplasty (THA), but melatonin may promote longer sleep sessions in the first few days after surgery, according to research presented at the AAOS 2025 Annual Meeting. Enhanced sleep may aid in recovery and improve patient satisfaction.
“In the first few weeks after surgery, nearly all patients have some degree of sleep disturbance. Despite its prevalence, there is limited evidence-based guidance on addressing these sleep disturbances,” said study coauthor Joshua C. Rozell, MD, FAAOS, associate professor in the Department of Orthopaedic Surgery at NYU Grossman School of Medicine. “To fill this gap, we evaluated melatonin, a safe and accessible supplement, to assess its potential role in improving sleep during the critical early recovery period after THA.”
The study assessed 139 patients who had primary, elective THA from July 2021 to March 2024. They were randomized to receive either 5 mg of melatonin (n = 75) or placebo (n = 64) every night for 14 days after surgery. Starting on the night of surgery (postoperative day 0 [POD0]) and for 14 consecutive days, patients used a diary to self-report the following factors:
- Pain on a visual analog scale (VAS)
- Number of hours slept
- Number of awakenings in the middle of the night
The researchers also assessed sleep disturbance preoperatively and on the 14th day after surgery (POD14) with the Patient-Reported Outcomes Measurement Information System Sleep Disturbance (PROMIS-SD) form, on which higher scores indicate greater sleep disturbance. To assess sleep quality, the research team used the Epworth Sleepiness Scale (ESS) on POD14 to assess sleep quality.
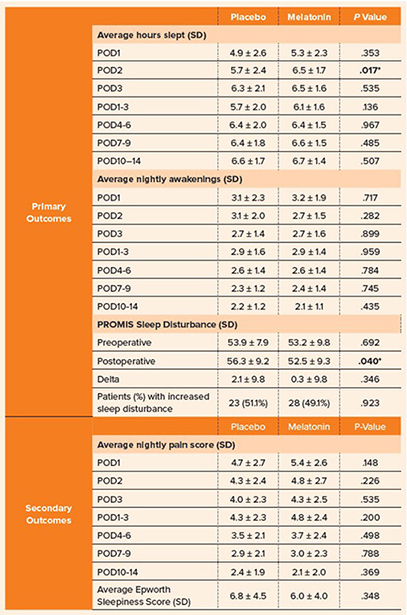
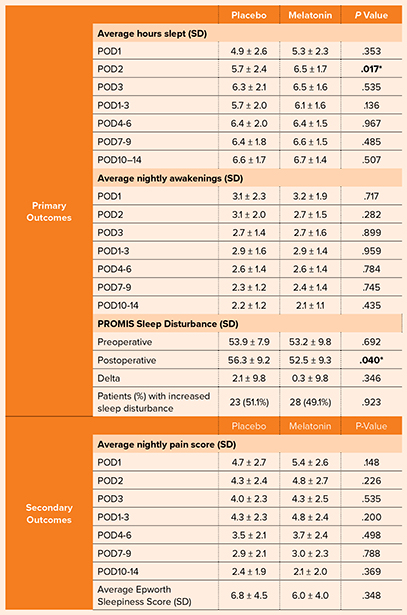
The study found that patients taking melatonin had significantly more hours of sleep on POD2 (melatonin: 6.5 ± 1.7 hours, placebo: 5.7 ± 2.4 hours, P = .017). They also averaged more sleep over POD1 to POD3 (melatonin: 6.1 ± 1.6 hours, placebo: 5.7 ± 2.0 hours, P = .136), but that finding was not statistically significant. The groups had comparable hours of sleep from POD4 to POD 14. Table 1 details the outcome scores between the melatonin and placebo groups.
Patients in the melatonin group also had fewer nighttime awakenings on POD2 (melatonin: 2.7 ± 1.5, placebo: 3.1 ± 2.0, P = .282), not a statistically significant finding.
They also had significantly lower postoperative PROMIS-SD scores (melatonin: 52.5 ± 9.3, placebo: 56.3 ± 9.2, P = .040). In addition, although not statistically significant, the melatonin group had lower postoperative ESS scores (melatonin: 6.0 ± 4.0, placebo: 6.8 ± 4.5, P = .348).
“We anticipated that melatonin would improve sleep duration and quality, given its sedative effect. However, we were surprised by the transient nature of its benefits, as sleep improvements were primarily observed only in the first three days following surgery,” Dr. Rozell said. “Additionally, while PROMIS-SD scores improved significantly, the lack of change in ESS scores was unexpected, suggesting that melatonin may have limited effects on overall daytime sleepiness. These findings underscore the complexity of postoperative sleep dynamics.”
The researchers plan to continue this line of inquiry by investigating the effects of higher doses of melatonin or extended use. They also are interested in assessing the long-term impact of improved sleep in the early postoperative period on key outcomes, including functional recovery, pain management, and overall patient satisfaction.
“Sleep plays a critical role in recovery after THA, and it’s important to address postoperative sleep disturbances as part of a comprehensive care plan,” Dr. Rozell said. “Melatonin offers a safe and effective intervention for early recovery, but it is not a one-size-fits-all solution. Instead, melatonin should be considered a component of a broader strategy tailored to each patient’s needs. We hope this work encourages greater awareness of the interplay between sleep and recovery and inspires continued research in this under-explored area.”
Dr. Rozell’s coauthors of “Does melatonin improve sleep following primary total hip arthroplasty: A randomized, double-blind, placebo-controlled trial” are Farouk Jarir Khury, MD; Muhammad A. Haider, BS; Kyle William Lawrence, BS; Thomas Christensen, BS; Stephanie A. Frezzo, MHA; Ran Schwarzkopf, MD, FAAOS; and William B. Macaulay, MD, FAAOS.
Keightley Amen, BA, ELS, is a freelance writer for AAOS Now.