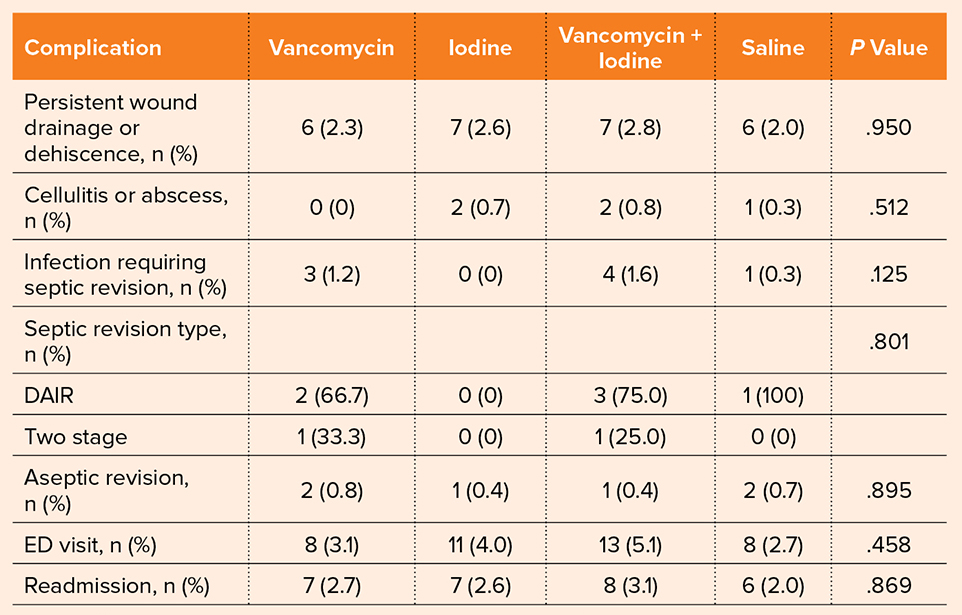
DAIR, debridement, antibiotics, and implant retention; ED, emergency department
A study presented at the AAOS 2025 Annual Meeting did not find significant differences between different measures for preventing periprosthetic joint infection (PJI) after total knee arthroplasty (TKA) in high-risk patients. The study was presented by Braden Saba, an orthopaedic surgery research fellow at NYU Langone Health in New York City and a medical student at Wake Forest School of Medicine in Winston-Salem, North Carolina.
The researchers conducted a multicenter, randomized trial comparing povidone iodine, topical vancomycin, and a combination of the two. In an interview for AAOS Now, Saba and coauthor Ran Schwarzkopf, MD, FAAOS, professor of orthopaedic surgery and associate director of the orthopaedic surgery residency program at NYU Grossman School of Medicine, shared the impetus for this study.
“Wound complications and PJI are two of the potentially disastrous complications of total joint arthroplasty. Some patients are at particularly high risk due to age, BMI, diabetes, immunocompromise, smoking, and more,” they explained. “To date, there has been no consensus on optimal joint irrigation prophylaxis for high-risk total joint arthroplasty patients. There are many techniques utilized [to reduce PJI risk], including iodine wash, vancomycin powder, saline lavage, and combinations therein, and we wanted to determine how much benefit each strategy offers from a wound complication and infection standpoint.”
The study included only high-risk patients, defined as age of 75 years or greater, BMI of ≥35 kg/m2 or greater, active smoker status, American Society of Anesthesiologists score of >2, immunosuppression, diabetes mellitus, or colonization with Staphylococcus aureus. In total, the study randomized 1,080 high-risk patients undergoing TKA.
There were four treatment groups: povidone iodine (three-minute soak) and topical vancomycin powder (2 g; n = 254), povidone iodine alone (n = 273), topical vancomycin powder alone (n = 256), or saline alone (n = 297). The researchers collected data on three-month wound complications, infections, and surgical outcomes.
“Ultimately, there are no clinical significant differences between prophylaxis techniques,” Mr. Saba and Dr. Schwarzkopf reported. “Wound complication and infection rates were comparably low in all groups, with no significant outliers.”
Table 1 details the rates of complications in each treatment group. Across all four groups, there were no differences in rates of persistent wound drainage or dehiscence (P = .95) or cellulitis or abscess (P = .51). Along with similar rates of infection at three months, the authors reported no difference in the type of septic revisions performed (P = .80). Aseptic revision rates were similar overall, along with emergency department visits and readmissions.
When asked whether they were surprised by the findings, Saba and Dr. Schwarzkopf said, “Intuitively, a ‘stronger’ antimicrobial prophylaxis technique (vancomycin powder plus dilute iodine wash) should lead to a clinically significant lower complication rate than saline lavage alone; however, we did not observe this difference. All groups performed comparably from an infection standpoint. This suggests that infection is a complex process that may require further research to better understand.”
One of the study’s limitations is that the low incidence rate of infection made it difficult to identify significant differences between prophylactic measures. However, according to the authors, “This study utilized biostatistician expertise along the way and determined that even if we increased our cohort size to 80,000, no clinical significant differences would emerge.”
Based on these findings, Dr. Schwarzkopf and Saba shared the following clinical takeaway for total joint surgeons: “Surgeon discretion can be used when deciding on intraoperative antimicrobial prophylaxis strategy in high-risk TKA.”
Regarding next steps, the authors shared that they will continue to follow these patients at one and two years postoperatively, “to ensure that this finding does not change with longer follow-up.”
They added, “It is important to keep in mind that our findings are only for the three-month timepoint following surgery; thus, further exploration is required to determine the longevity of this finding.”
Mr. Saba’s and Dr. Schwarzkopf’s coauthors of “Three-month wound complication and infection rates after vancomycin powder and dilute povidone iodine lavage for infection prophylaxis in high-risk total knee arthroplasty: A multicenter randomized control trial” are Adriana P. Liimakka; Alex Tang, MD; Alison K. Klika; Amethia D. Joseph, MHA; Anne Debenedetti, MSc; Antonia F. Chen, MD, MBA, FAAOS; Brett R. Levine, MD, MS, FAAOS; Carlos A. Higuera Rueda, MD, FAAOS; Daniel Waren, MSPH; Douglas A. Dennis, MD, FAAOS; Dylan Oliver, MD; Eileen Poletick, DNP, RN; Farouk J. Khury, MD; Gregory J. Schneider, MD; Hayley E. Raymond, BA; Herbert J. Cooper, MD, FAAOS; Ian S. Hong, MD; Ignacio Pasqualini, MD; James C. Wittig, MD, FAAOS; Jesus M. Villa, MD; John M. Dundon, MD, FAAOS; Joshua B. Davis, BS; Joshua C. Rozell, MD, FAAOS; Martin Malik; Mia J. Fowler, BS; Morteza Meftah, MD; Nickelas Huffman, BS; Nicolas S. Piuzzi, MD; Olivia P. Vyge, MSc; Paul M. Lombardi, MD; Richard S. Yoon, MD, FAAOS; Roseann M. Johnson, BS, CCRP; Stephen R. Rossman, DO, FAAOS; Vinay Aggarwal, MD, FAAOS; Vladimir Tress, MD; Walter L. Taylor, MS, BS; William J. Long, MD, FAAOS; William B. Macaulay, MD, FAAOS; Yair D. Kissin, MD, FAAOS; Yibin B. Zhang, BA; Zeynep Seref-Ferlengez, PhD; and Zoe Alpert.
Rebecca Araujo is the managing editor of AAOS Now. She can be reached at raraujo@aaos.org.