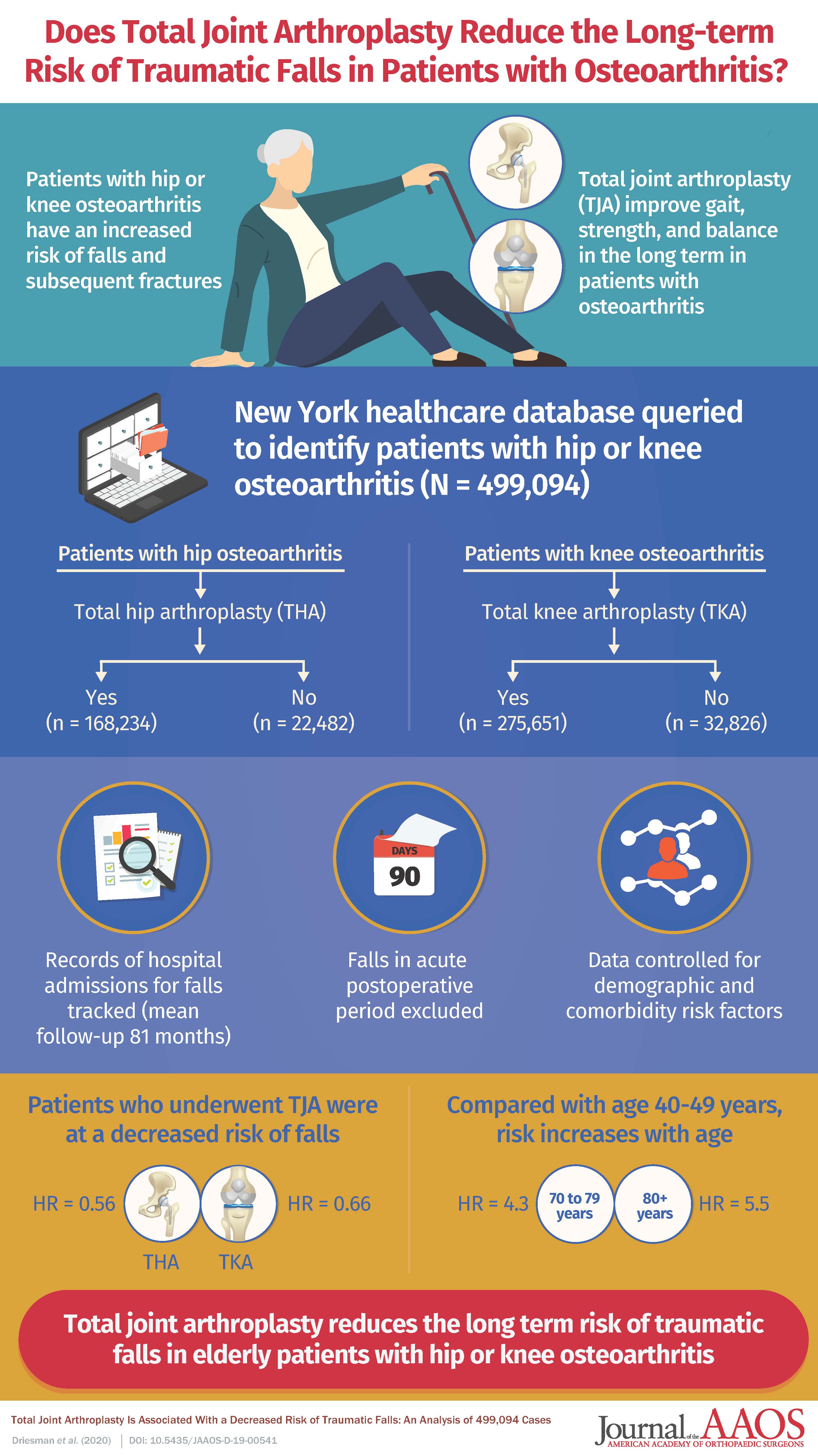
ROSEMONT, Ill. (October 16, 2020)—Patients who have had a total joint arthroplasty (TJA) demonstrate excellent long-term outcomes with increased mobility and improved ability to complete their activities of daily living. However, there is still an ongoing debate whether patients who have undergone TJA are at an increased risk of falls and fragility fractures. According to a new research article published in the Journal of the American Academy of Orthopaedic Surgeons®, authors compared the fall rates of nearly 500,000 cases of osteoarthritic patients and found those who underwent TJA experienced a significantly lower number of falls post-op than those who did not have the surgery.
“Osteoarthritis (OA) is the degeneration of the cartilage in our joints over the years,” said lead author and orthopaedic surgeon Ran Schwarzkopf, MD, FAAOS. Dr. Schwarzkopf specializes in adult reconstruction in the Department of Orthopedic Surgery at NYU Langone Health. “As the wear and tear increases, patients lose their range of motion. They cannot turn their toes as easily, flex their hips or lift their legs high enough to avoid obstacles due to physical limitations as well as pain, resulting in falls and fragility fractures.”
In this data-driven study, Dr. Schwarzkopf and his research colleagues used the Statewide Planning and Research Cooperative System (SPARCS) New York database to separate patients with the primary diagnosis of lower extremity osteoarthritis into four categories. Patients with hip OA who underwent TJA were compared to patients with hip OA who did not undergo TJA, while patients with knee OA who underwent TJA were compared to patients with knee OA who did not undergo TJA. The fall rates, determined by the number of hospital visits reporting fragility fractures in the two years after OA diagnosis in patients who opted not to have surgery were significantly higher than the fall rates of OA patients who underwent TJA in the two years after the surgery.
Patients from the database were grouped by age and various other demographics to ensure accuracy. Cases were also tracked longitudinally for up to two years after surgery. In order to avoid the bias of post-op recovery time, the first few months after surgery were eliminated from the study.
“We looked at how many people from each group came into a hospital to seek care for their fragility fracture, due to a fall, and found that those who had TJA fell far less than those who did not. From that, we concluded that TJA for patients that have OA is protective against future falls,” Dr. Schwarzkopf added.
Research shows that TJA is known to decrease pain, increase range of motion and agility and lead to a more successful physical therapy program for lower extremity OA patients. Mentally, patients who have TJA performed also experience less fear of falling, leading to more stability and confidence in their daily movements.
“TJA will allow patients to go back to the daily activities they may have avoided due to pain and restricted range of motion,” explained Dr. Schwarzkopf. “They are able to go back to the point in their lives when they can do activities, such as hiking, riding a bicycle or even walking their dog, without having to think about whether it will cause them physical pain or rely as heavily on ambulatory aids and caregivers.”
While the research was focused on how to resolve arthritis and improve quality of life for patients, Dr. Schwarzkopf notes not everyone needs to have a joint replacement surgery. Symptoms of OA can be treated with anti-inflammatory medication, walking aids and exercises to increase strength. Only when patients are unable to continue to live with the symptoms of OA despite undergoing conservative treatment and they understand the risks and recovery of TJA is the surgery recommended.
Whether patients choose TJA surgery or opt to use alternative methods for symptom management, an at-home caregiver can be vital to keeping OA patients safe from falls. In anticipation of November being National Family Caregivers Month, Dr. Schwarzkopf offers the following tips to help caregivers keep patients or loved ones with OA safe from falls:
- Cover sharp corners of tables or counters
- Remove loose rugs from the patient’s primary routes
- Install handrails to bathrooms and staircases
- Use motion-activated nightlights
- Encourage the use of wearable or portable communication devices in case of falls
For more information about osteoarthritis and treatment options, visit OrthoInfo.org, the authoritative, trusted consumer website on bone and joint health. To schedule an interview about this JAAOS® review article, email media@aaos.org.
# # #
More information about the AAOS
Follow the AAOS on Facebook, Twitter and Instagram.
Follow the conversation about JAAOS on Twitter.
Contact AAOS Media Relations
Deanna Killackey
847-384-4035
killackey@aaos.org
Lauren Riley
847-384-4031
pearson@aaos.org